Scientists investigating the potential of combined and more powerful drug treatments have found that antimicrobial resistance to these is arising via the vitamin B2 synthesis pathway.
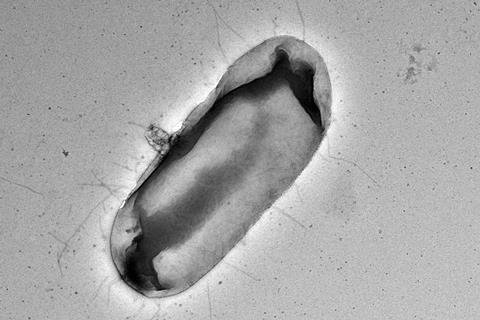
A new study from scientists at Massey University, Palmerston North, New Zealand, revealed that bacteria gain resistance to furazolidone and the furazolidone-vancomycin synergy through novel mutations in the riboflavin (vitamin B2) biosynthesis pathway.
Corresponding author Van Hung Vuong Le, a junior editor with Letters in Applied Microbiology, an Applied Microbiology International publication, said that some of the mutations studied actually enhanced bacterial growth at sub-lethal levels of drug treatment.
The study, ‘Mutations in the riboflavin biosynthesis pathway confer resistance to furazolidone and abolish the synergistic interaction between furazolidone and vancomycin in Escherichia coli’ is published in Microbial Genomics.
Drug discovery slowing
“Antibiotic resistance, particularly amongst Gram-negative pathogens, is a major concern, and the discovery of new antibiotics has slowed dramatically. Therefore, additional options need to be explored, such as antibiotic combinations,” said Dr Le.
“Synergistic combinations - whose antibacterial effect is stronger than when used alone - are a promising way to expand treatment options. The combination of furazolidone and vancomycin is one such example we have shown in our previous studies.
“This work investigated the resistance mechanisms that can arise in E. coli towards the furazolidone-vancomycin combination, which would inform treatment and dosing strategies for this combination.”
Synergistic interaction
Vancomycin and furazolidone are two approved antibiotics - vancomycin is only efficient against Gram-positive bacteria, while furazolidone is a representative of the nitrofuran pro-drug class, “an old drug group” that has gained traction for use as first line therapy.
READ MORE: Antibacterial material restores the efficacy of antibiotics against resistant bacteria
READ MORE: The effect of combinations of antibiotics and natural products on antimicrobial resistance
The Rakonjac lab has previously reported and characterized the synergistic interaction between vancomycin and furazolidone against Escherichia coli. In this case, they investigated the mechanism of bacterial resistance to the synergistic furazolidone-vancomycin combination that would lay foundations for clinical use of this combination.
“Interestingly, while selecting for resistant mutations on the antibiotic combination treatment, we found novel mutations to furazolidone in the riboflavin biosynthesis pathway (e.g., ribB and ribE genes), that are unlikely to be isolated if selection on the furazolidone treatment alone,” Dr Le said.
“We then figured out the mechanism of action mediated by these ribB/ribE mutations, in which these mutations cause a decrease in the furazolidone activation rate, and therefore diminish the furazolidone antibacterial activity and the furazolidone-vancomycin synergistic interaction.”
Isolated mutants
The team selected E. coli mutants that are resistant to the furazolidone-vancomycin synergistic combination treatment and characterised them both phenotypically and genetically. All the isolated mutants showed a decrease in the synergy between furazolidone and vancomycin compared to the parental strain.
Using whole genomic sequencing to detect genetic changes in the isolated mutants, they found that all the strains that displayed increased furazolidone resistance had a mutation in either the ribB or ribE genes, two essential genes in the riboflavin (vitamin B2) biosynthesis pathway.
The mechanism of why the ribB/ribE mutations caused furazolidone resistance and the loss of the drug synergistic interaction were further investigated using genetic knock-out mutants and checkerboard assays. The researchers found that these ribB/ribE mutations exert their effect through decreasing the cellular nitroreductase activity that is responsible for activating nitrofuran antibiotics, including furazolidone.
Unexpected outcome
“A common thought would be that adding riboflavin to the medium could complement the disrupted riboflavin biosynthesis pathway to make the furazolidone-resistant ribB/ribE mutants sensitive to furazolidone again and may be used as an antibiotic enhancer. We showed an unexpected outcome: Addition of riboflavin revert their growth defect caused by the ribB/ribE mutants but did not restore sensitivity to furazolidone,” Dr Le said.
The ribE in-frame four-residue deletion mutant, which displayed the growth defect, showed greatly improved growth at sub-lethal concentrations of furazolidone. Basically, the antibiotic did not kill but instead enhanced bacterial growth in this scenario.
“In the present work, we selected this specific ribE mutation upon the antibiotic exposure in the laboratory. Nonetheless, by searching the public sequencing database, some multidrug resistant clinical isolates were found to have this same mutation and hence the exact same mutants are already circulating out there in nature,” Dr Le said.
“Mutations in ribE have been previously linked to nitrofuran resistance and are included when surveying nitrofuran resistance, however our findings suggest that mutations in ribB should also be included.
Large fitness cost
“Our findings also explain why the ribE gene mutations may arise in the clinical setting despite a large fitness cost to the host, likely due to their ability to regain wild-type growth levels in the presence of riboflavin, whilst retaining a furazolidone-resistant phenotype and/or being co-selected with other antimicrobial resistance genes.
“Given that nitrofurans have been commonly used for urinary tract infection therapy in recent years, ribE mutants are expected to become a formidable obstacle in the treatment of infections caused by multi-resistant Gram-negative pathogens.
“Further investigation is required into why supplementation with riboflavin restores the ribB/ribE mutant growth but does not restore the furazolidone sensitivity. In addition, further investigation is required into why the ribE mutants’ growth is improved at sublethal concentrations of furazolidone.”
Background to research
The work was conducted by Hannah Wykes during her Masters research at Massey University. She currently works at New Zealand Pharmaceuticals Ltd. The project was supervised by Professor Jasna Rakonjac at the School of Food Technology and Natural Sciences, Massey University, Palmerston North, New Zealand, and co-supervised by Dr. Vuong Le, originally a postdoctoral researcher at Massey University and currently at the Living Systems Institute, University of Exeter, Exeter, UK.
The work was supported by the Massey University School of Food Technology and Natural Sciences and Generous donation by Anne and Bryce Carmine to JR laboratory. HW was supported by a Graduate Women Manawatū Charitable Trust and the William Georgetti Scholarship.
Topics
- Antibiotics
- Antimicrobial Resistance
- Applied Microbiology International
- Asia & Oceania
- Bacteria
- Community
- Early Career Research
- furazolidone
- Hannah Wykes
- Infection Prevention & Control
- Jasna Rakonjac
- Massey University
- New Zealand Pharmaceuticals Ltd
- nitrofuran
- One Health
- Pharmaceutical Microbiology
- Research News
- riboflavin biosynthesis pathway
- synergistic interactions
- UK & Rest of Europe
- university of exeter
- Van Hung Vuong Le
- vancomycin







No comments yet