Scientists from The University of Texas Health Science Center at San Antonio (UT Health San Antonio) co-led a global research team that discovered the answer to a long-standing question in malaria research: Do people who live in areas where malaria is ever-present develop broadly neutralizing antibodies against the malaria parasite? The answer is yes, as presented in a study published Nov. 20 in the journal Nature.
“Our study shows for the first time how antibodies can protect against severe malaria and provides new insights into prevention and treatment of this often-fatal disease,” said co-senior author Evelien M. Bunnik, PhD, associate professor in the Department of Microbiology, Immunology & Molecular Genetics, Joe R. and Teresa Lozano Long School of Medicine at UT Health San Antonio.
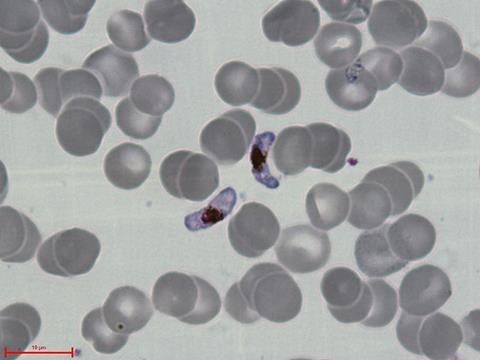
The team, comprised of scientists from the United States, Denmark, Spain, Tanzania and Uganda, explored how immunity develops against Plasmodium falciparum, the parasite that causes the most severe forms of malaria. They found that broadly reactive antibodies from various individuals consistently bound to the same site on a key virulence protein of the malaria parasite.
Tragically common, deadly disease
Malaria is caused by a parasite transmitted to humans by mosquitoes and is especially prevalent in tropical parts of Africa and South Asia. The Centers for Disease Control and Prevention reported in 2023 there were approximately 250 million malaria cases globally, resulting in 600,000 deaths, with 95% of deaths occurring in Africa.
READ MORE: Malaria parasite generates genetic diversity using evolutionary ‘copy-paste’ tactic
READ MORE: Human antibodies could prevent the malaria parasite from causing life-threatening infections
Bunnik said treating a parasite, like the one that causes malaria, can be much more challenging than treating a virus. This parasite has a complex life cycle where it can infect a person in one form and then evolve to a different form, expressing different antigens.
“The immune response against one form of the parasite does nothing against another form,” she said. “As the parasite goes through its lifecycle, it shapeshifts and becomes a completely different target for the immune system.”
Skilled enemy
Another challenge is that the malaria parasite has evolved for tens of thousands of years alongside humans and non-human apes and is now highly adapted to escaping our immune responses.
“People infected with malaria parasites can make a very strong immune response, but the parasite has ways to deal with that and escape,” she said.
An effective malaria vaccine is challenging, in part due to the enormous variation in the parasite’s virulence genes that play an important role in the disease process. This study shows that the parasite has a weakness, however, because a specific site on its polymorphic erythrocyte membrane protein 1 (PfEMP1) protein must bind to a protein receptor of the human host, called endothelial protein C receptor (EPCR), for severe malaria to develop. Antibodies that target this binding site neutralize the parasite’s virulence, making it an ideal focus for vaccine development.
“This epitope represents an Achilles’ heel of the parasite, as it cannot be altered without the parasite losing its ability to bind to the human receptor EPCR,” Bunnik said.
Achilles heel
Samples from Ugandan individuals showed that two human monoclonal antibodies could bind and inhibit many different variants of PfEMP1. Serum samples from Tanzanian adults and children showed that antibodies targeting the EPCR binding site of PfEMP1 are common for individuals continuously exposed to the malaria parasite and develop early in life, in children between 2 and 9 years old.
A three-dimensional human microvasculature model created by the team in Spain demonstrated that these particular antibodies successfully inhibited the binding of malaria parasite-infected erythrocytes to the human endothelial cells that line blood vessel walls.
The various teams are now furthering their malaria research based on findings from this study.
Bunnik’s lab will continue the search for monoclonal antibodies against PfEMP1 and is specifically looking for antibodies that recognize additional EPCR-binding subclasses. She is also interested in answering the question of how such antibodies develop.
“If we activate the human endothelium that’s present in these microvessels, does it have an effect on parasite binding and do our antibodies still inhibit it?” Bunnik said. “And if we add antibodies that inhibit parasite binding to these other receptors, do we get a synergistic effect?”
Collaborative effort
The lead author for the study is Bunnik’s former mentee Raphael Reyes, PhD, who graduated last year from the Integrated Biomedical Sciences program with the UT Health San Antonio Graduate School of Biomedical Sciences. He is currently working on his post-doctoral fellowship at the Ragon Institute of Mass General, MIT and Harvard in Cambridge, Massachusetts.
The team in Spain who created the microvasculature model for this study are continuing research to further understand how these antibodies inhibit the malaria parasite’s binding to the endothelium.
The findings of this study provide a pathway for a malaria vaccine that mimics the naturally acquired immunity seen in populations that are continually exposed to the parasite. Bunnik said the team is working on the framework for potential vaccines with experts in computational protein design.
“Now that we know what the epitope looks like, we can try to scaffold that in different ways onto other proteins, assisted by computational predictions and present it to the immune system in a way that is highly immunogenic,” she said.







No comments yet