More than 200 viruses can infect and cause disease in humans; most of us will be infected by several over the course of a lifetime. Does an encounter with one virus influence how your immune system responds to a different one? If so, how? Does it weaken your defenses, boost them, or have some other impact altogether?
These are questions Rockefeller University scientists from the Laboratory of Virology and Infectious Disease,headed by Charles M. Rice, and Weill Cornell Medicine’s Laboratory of Epigenetics and Immunity, headed by Steven Z. Josefowicz, teamed up to answer in a new study published in the journal Immunity.
READ MORE: Long Covid continues to evade diagnosis
READ MORE: Obesity may increase susceptibility to contracting COVID-19
By analyzing mice that had been first infected with and then with influenza A virus, the scientists found that having recovered from COVID had a protective effect against the worst effects of the flu, and that this memory response was coming from an unexpected corner of the immune system.
Antiviral immune memory in macrophages
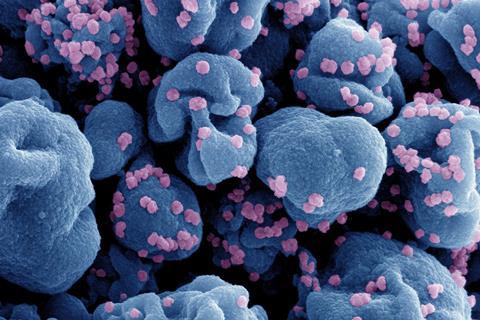
It turned out that epigenetic changes in macrophages—innate immune cells that are among the first responders to a threat—had developed a kind of “memory” following COVID that allowed these cells to mount a better defense against an unrelated virus. Immunological memory has long been thought to be limited to adaptive immune cells, though recent work has challenged this dogma. More intriguingly, what macrophages were remembering wasn’t unique to any particular virus.
The findings increase our understanding of innate immune memory and may enable researchers to exploit the phenomenon in new ways to create therapies that confer widespread protection against multiple viruses.
“Immune memory is critical to fending off recurring diseases caused by pathogens. What’s exciting about our study is that we’ve discovered a broadly effective antiviral immune memory in macrophages following SARS-CoV-2 infection that can reduce disease caused by a completely different virus,” says first author Alexander Lercher, a postdoctoral fellow in the lab.
“A more detailed understanding of these mechanisms could aid development of new therapeutic strategies the cover a range of respiratory viruses,” says Rice.
“It was so exciting to team up with Alex and Charlie and delve into the epigenetic mechanisms encoding this general antiviral memory,” adds Josefowicz. “The implications are profound. If we can walk around with months-long bolstered immunity after a season’s worth of respiratory infections, what are the implications for seasonal trends in these infections? How much human variance—genetic and epigenetic—exists in these pathways?”
Cascading effect
When a virus invades the body, signaling molecules called cytokines instruct innate immune cells like macrophages to pursue and consume anything that sounds their alarm. This one-size-fits-all approach is followed by a targeted assault by adaptive immune cells such as T cells, which identify a virus-specific antigen, tailor their offense towards it, and remember it long-term to fight future invasions by the same virus.
However, discoveries of the past two decades show that innate immune responses can lead to cellular memory. In multiple studies, for example, researchers discovered that people who had received the Bacillus Calmette-Guérin live-attenuated vaccine, which aims to protect against tuberculosis, elicited innate immune memory responses that last for months, and provide protection against unrelated infections.
But how this broadly effective immune memory develops is little understood. In 2020, Lercher began investigating the phenomenon using widely circulating viruses: SARS-CoV-2, then the most dominant global pathogen, and influenza A virus, a recurrent scourge plaguing humanity since the 1918 pandemic, when it crossed from birds to humans, spreading globally and killing millions.
Flipping the switch on genes
Lercher and colleagues set out to investigate long-term consequences of past SARS-CoV-2 infection in the respiratory system. They focused their analysis on cells in the lungs and found that alveolar macrophages, located in the airway, acquired a new epigenetic program after infection. More specifically, they found that the chromatin that packages genes was more accessible around antiviral genes, which rendered them “ready to go” following recovery from COVID.
These results weren’t limited to mice. When analyzing samples from people who’d recovered from mild COVID, the researchers found similar epigenetic changes in monocytes in the blood, the progenitor cells of macrophages.
The result of this epigenetic reprogramming is memory of previous infections—and an altered immune response to future ones.
Sharp memory
Because macrophages in the lungs of COVID-recovered mice had acquired antiviral innate immune memory imprinted on their chromatin, they could more successfully fight disease caused by a new viral invader. Compared to naive mice, they had fewer disease symptoms from influenza A, such as significant weight loss or dysregulated inflammatory responses, and lower mortality rates.
“The fact that viral RNA alone seems to be able to trigger memory in macrophages lays the foundation of this memory being antigen independent,” Lercher says. “They’re recognizing a pattern that is shared by many viruses, unlike a virus-specific antigen.”
The researchers confirmed this by exposing mice to a synthetic mimic of an RNA virus, and found similar memory responses as they had seen following SARS-CoV-2 infection.
Interestingly, when it came to battling the secondary flu infection, memory-attuned macrophages outperformed adaptive T cells. “The macrophages are really the ones driving this response,” Lercher says.
Finally, to test how sharp the macrophages’ memory was, the researchers extracted them from recovered mice, transferred them into naive mice and then infected those mice with influenza A virus. So, if the recovered macrophages were up to the task, the recipient mice should develop less severe disease upon influenza A infection.
They were. “The naive mice with the implanted recovered macrophages fared better against influenza than mice implanted with naive macrophages,” Lercher says.
Pandemic preparedness
In the future, the researchers want to identify what the critical factors for establishing innate immune memory are. “In an ideal world, we would find one or a few factors that lead to this memory formation in macrophages and other innate cells, and then exploit it to develop therapies that offer broad protection against many viruses,” Rice says.
This approach could be especially useful in the face of a potential pandemic. “If there were a new emerging pathogen on the horizon, for example, it would be nice to have a therapy that boosted your general antiviral immunity for the next month or so,” says Lercher. “That’s still very far away, and a lot more research needs to be done, but I think it could be possible one day.”







No comments yet