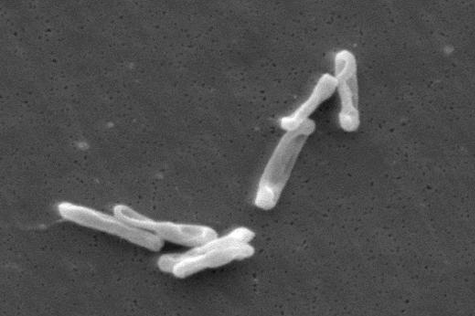
Clostridioides difficile (C. difficile) infection (CDI) is a significant healthcare-associated infection, known for its high morbidity and mortality rates, especially in vulnerable populations. CDI presents in a wide range of severity, from mild diarrhea to life-threatening complications like toxic megacolon. Risk factors include antibiotic use, advanced age, immunosuppression, and various comorbidities such as liver disease and diabetes.
Recurrence is a major concern, with 20% to 30% of patients experiencing it within two weeks after treatment, and this rate increases with multiple episodes. The emergence of hypervirulent strains like BI/NAP1/027 and advances in diagnostic tools have increased the incidence and severity of CDI, prompting new treatment strategies.
The treatment of CDI has evolved, particularly for non-severe cases. Both fidaxomicin and oral vancomycin are now recommended for initial treatment, with fidaxomicin preferred due to its ability to reduce recurrence. Fidaxomicin, a macrolide antibiotic, offers a narrower spectrum of activity, preserving the gut microbiome and reducing toxin re-expression, which translates into improved clinical outcomes and lower recurrence rates. Oral vancomycin, while effective, remains a second-line option in some guidelines due to its broader spectrum. Despite these advances, the high cost of fidaxomicin limits its use in certain settings.
READ MORE: Synthetic microbiome therapy suppresses bacterial infection without antibiotics
READ MORE: mRNA vaccine created to prevent and treat C. difficile
For severe CDI, defined by criteria like elevated white blood cell count or kidney dysfunction, both fidaxomicin and vancomycin are recommended, though the choice of treatment remains under debate. While vancomycin is commonly used, there is no conclusive evidence to suggest a preference for fidaxomicin in severe cases. For fulminant CDI, a more aggressive approach is needed, involving high-dose vancomycin and intravenous metronidazole. Fecal microbiota transplantation (FMT) is considered in refractory cases of severe or fulminant CDI.
Fecal Microbiota Transplantation (FMT)
FMT has emerged as a key treatment for recurrent CDI (rCDI), showing significant success in restoring gut microbiome diversity and preventing recurrence. Conventional FMT involves transferring fecal matter from a healthy donor to the patient, typically via colonoscopy or enema. Newer live biotherapeutic products (LBPs) like Rebyota and Vowst offer promising alternatives by delivering purified microbial formulations. Both products have demonstrated efficacy in reducing CDI recurrence, particularly for patients with multiple recurrences. However, FMT’s application remains selective, with some guidelines recommending it only after multiple episodes or in severely ill patients.
Treatment of recurrent CDI (rCDI)
For patients with rCDI, fidaxomicin is preferred due to its lower recurrence rate compared to vancomycin. Extended-pulsed fidaxomicin, which involves a tapered dosing regimen, has shown promising results in reducing recurrence. Additionally, rifaximin is considered a follow-up therapy after vancomycin, particularly in patients with multiple recurrences. Bezlotoxumab, an IgG1 monoclonal antibody targeting C. difficile toxin B, is recommended for high-risk patients to prevent further recurrences. While the addition of bezlotoxumab has shown benefit in reducing recurrence, its high cost remains a barrier in some healthcare settings.
Emerging Strategies for CDI Prevention and Treatment
Several emerging strategies offer hope for better managing CDI and its recurrences. Vaccines and bacteriophage therapies are being explored as alternatives to antibiotics, aiming to prevent CDI without disrupting the gut microbiome. Though some early-stage vaccine trials have shown promise in reducing CDI symptoms, the lack of significant efficacy in large trials means vaccines are not yet a viable widespread solution. Bacteriophage therapy, which targets specific bacteria without harming the microbiome, is still under investigation but may become a future option for CDI treatment.
Artificial intelligence (AI) and predictive risk models also hold promise for early detection and prevention. Machine learning algorithms are being tested to predict the risk of CDI in hospitalized patients, offering the potential for timely interventions and more targeted treatment strategies.
Conclusion
Clostridioides difficile infection remains a critical challenge in healthcare, with recurrence being a major complication. Current treatments like fidaxomicin and vancomycin, along with newer therapies like FMT and bezlotoxumab, offer effective solutions, particularly for recurrent or severe cases. Emerging treatments, including vaccines, bacteriophages, and AI-based risk models, offer exciting prospects for better management and prevention of CDI. However, ongoing research and clinical trials are essential to refine these therapies, address cost concerns, and establish optimal treatment protocols for diverse patient populations.
Topics
- Artificial Intelligence & Machine Learning
- Bacteria
- Bezlotoxumab
- BI/NAP1/027
- Clostridioides difficile
- fidaxomicin
- Gut Microbiome
- Healthy Land
- IgG1 monoclonal antibody
- Infection Prevention & Control
- live biotherapeutic products (LBPs)
- One Health
- Phage Therapy
- recurrent Clostridioides difficile infection
- rifaximin
- toxic megacolon
- USA & Canada
- Vaccinology
- vancomycin







No comments yet