Respiratory syncytial virus (RSV) is a leading cause of lower respiratory tract infections in children under two years old, resulting in significant morbidity and a heavy economic burden on healthcare systems worldwide. Despite its widespread prevalence, the relationship between respiratory bacteria and RSV infection has remained underexplored.
The interactions between viruses and the microbiome—especially in the early stages of infection—are critical, as they can influence immune responses and disease outcomes. However, studies have shown varying results regarding how specific bacterial profiles affect RSV severity, indicating the need for more comprehensive research to clarify these complex dynamics.
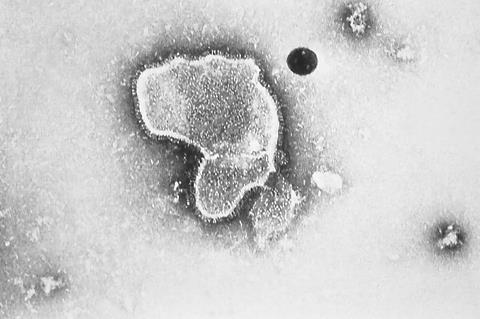
A new scoping review, led by the Children’s Hospital of Chongqing Medical University and published in Pediatric Discovery, examines the impact of respiratory bacteria on the severity of respiratory syncytial virus (RSV) infections and long-term health outcomes in children.
By synthesizing data from 33 studies, researchers found that specific bacterial profiles, including Streptococcus pneumoniae and Haemophilus influenzae, significantly influence the severity of RSV infections and the risk of developing recurrent wheezing or asthma. The study highlights the importance of understanding the interactions between respiratory viruses and bacteria, offering insights for potential therapeutic strategies to improve outcomes for children affected by RSV.
Bacterial colonization in children’s respiratory tracts impacts RSV infections
The review identifies several key bacterial species prevalent in the respiratory tracts of children with RSV infections, including Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Staphylococcus aureus. These bacteria were found to have significant effects on both short-term and long-term RSV outcomes.
Haemophilus influenzae, for example, was consistently associated with more severe disease, longer hospital stays, and higher rates of ICU admissions. In contrast, Streptococcus pneumoniae showed mixed results: while some studies linked it to more severe RSV infections, others suggested that higher bacterial densities might actually provide a protective effect, reducing the risk of severe disease. These findings highlight the complex and sometimes contradictory relationship between bacterial colonization and RSV infection outcomes.
READ MORE: Researchers identify signs tied to more severe cases of RSV
READ MORE: Scientists pinpoint new drug target for RSV
Long-term consequences of these bacterial profiles were also evident in the study, with certain bacteria influencing the development of recurrent wheezing or asthma. For instance, the presence of Lactobacillus was associated with a reduced risk of childhood wheezing, while higher levels of Moraxella catarrhalis and Streptococcus pneumoniae correlated with an increased risk of recurring wheezing episodes.
These results emphasize the critical role of the respiratory microbiome in shaping both the acute and chronic phases of RSV infection, suggesting that modulating bacterial profiles could be an important therapeutic approach to mitigate disease severity and prevent long-term respiratory complications.
Limitations and future implications
Dr. Yu Deng, the corresponding author of the study, stressed the complexity of the findings and the need for further research: “Our study underscores the pivotal role that respiratory microflora play in shaping RSV infection outcomes. However, the inconsistent findings also reflect the intricate nature of host-microbe interactions. More targeted research is essential to fully understand these dynamics and develop effective interventions.”
The implications of this research for pediatric healthcare are profound. By elucidating the impact of specific bacterial profiles on both the severity of RSV infections and their long-term health consequences, the study paves the way for potential new strategies in prevention and treatment.
Interventions that modify the respiratory microbiome could help reduce the severity of RSV infections and potentially prevent the development of chronic conditions like asthma. Moving forward, continued research into the mechanisms behind these microbial interactions holds the promise of microbiome-based therapies that could transform the management of RSV and other respiratory diseases in children.
Topics
- Asia & Oceania
- Bacteria
- Children’s Hospital of Chongqing Medical University
- Disease Treatment & Prevention
- Haemophilus influenzae
- Healthy Land
- Lung Microbiome
- Moraxella catarrhalis
- One Health
- Research News
- respiratory syncytial virus
- Staphylococcus aureus
- Streptococcus pneumoniae
- Taxonomy, Phylogeny, Function
- Viruses
- Yu Deng







No comments yet