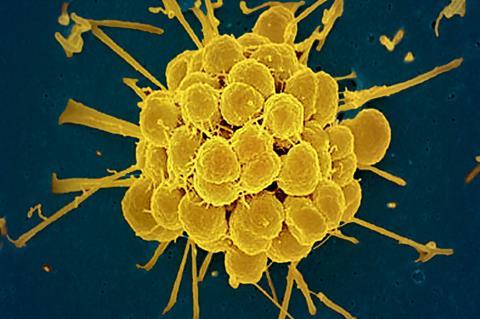
Antimicrobial resistance (AMR) is one of the most pressing public health challenges of the 21st Century. One area of particular concern is AMR gonorrhea, a potent strain of the sexually transmitted bacteria that has become resistant to all of the antibiotics once used to treat it.
In response to this public health threat, health officials in the United States established the national Gonococcal Isolate Surveillance Project (GISP) to monitor the prevalence of AMR gonorrhea in 25-35 sites across the country annually. But that data, while intended to be representative for the U.S., leaves large swaths of the country unaccounted for when it comes to localized infections.
A new study led by researchers at the Yale School of Public Health could help fill those data gaps and significantly improve AMR gonorrhea surveillance nationally. The study, published in the journal Lancet Regional Health – Americas, identifies specific geographical locations and population characteristics—including population density and HIV prevalence—associated with the spread of AMR gonorrhea. The findings could help focus future prevention and treatment efforts where they are needed most.
Prevalence of AMR gonorrhea - geograpgical factor
Using data from the national GISP, the study examined the association between various population-level characteristics and the prevalence of AMR gonorrhea across the United States between 2000 and 2019. The researchers analyzed more than 112,000 bacteria cultures collected from 30 cities to determine the prevalence of resistance to three common antibiotics used to treat gonorrhea—ciprofloxacin, penicillin, and tetracycline.
READ MORE: CARB-X funds Visby Medical to develop a portable rapid diagnostic for gonorrhea
READ MORE: Unlikely ally: sex hormones help gonorrhea fight off antimicrobials and antibiotics
One of the most important findings was that the prevalence of AMR gonorrhea varies significantly in different parts of the country. According to the study, cities in the Southeast and Western parts of the United States (Honolulu, San Diego, San Francisco, Orange County, and Seattle) had the highest rates of the resistant strain, while those in the Northeast had the lowest.
Prevalence of AMR gonorrhea - population density
In addition to geographic factors, population density played a significant role in the spread of AMR gonorrhea. The study found that denser populations were associated with a 50% increase in the likelihood of resistance to ciprofloxacin and a 36% increase in resistance to penicillin. This suggests that urban centers with high population concentrations are hot spots for the spread of the pathogen.
“These findings underscore the need for targeted public health interventions in specific regions and urban areas,” said Dr. Reza Yaesoubi, PhD, an associate professor of public health (health policy) at the Yale School of Public Health and one of the study’s senior authors. “By understanding the local risk factors for antimicrobial resistance, we can prioritize surveillance and treatment efforts in areas where they are most needed.”
Surveillance of AMR gonorrhea spread
The study also highlights the association between AMR gonorrhea and the prevalence of HIV. An increase in HIV cases was linked to higher resistance to ciprofloxacin and tetracycline, indicating that AMR gonorrhea could be more prevalent in communities with higher rates of sexually transmitted infections (STIs).
“This research can help inform local policymakers so they can allocate resources effectively,” Yaesoubi said. “Expanding surveillance in cities with dense populations and high HIV prevalence could help monitor the spread of resistant gonorrhea more accurately and allow health officials to respond to rises in antimicrobial resistance more promptly.”
The study suggests that expanding surveillance programs like GISP to more cities, particularly in regions identified as high-risk, could improve the detection and treatment of AMR gonorrhea. Policymakers might also consider conducting routine drug susceptibility tests in these areas to ensure patients receive the most effective treatment.
Yale School of Public Health (YSPH) Associate Researcher, Jingwen Li, MPH ’22, is the study’s lead author and YSPH Associate Professor of Biostatistics Joshua L. Warren is co-senior author. Other authors on the study are Rachel E. Murray-Watson from the Yale School of Public Health’s Public Health Modeling Unit; Sancta B. St. Cyr, from the U.S. Centers for Disease Control and Prevention’s Division of STD Prevention; and Yonatan H. Grad, of the Department of Immunology and Infectious Diseases at Harvard T. H. Chan School of Public Health and Brigham and Women’s Hospital’s Division of Infectious Diseases.
Topics
- AMR gonorrhea
- Antibiotics
- Antimicrobial Resistance
- Bacteria
- Brigham and Women’s Hospital’s Division of Infectious Diseases
- Gonococcal Isolate Surveillance Project
- Harvard T. H. Chan School of Public Health
- Healthy Land
- Jingwen Li
- Joshua L. Warren
- One Health
- Rachel E. Murray-Watson
- Research News
- Reza Yaesoubi
- Sancta B. St. Cyr
- The Sex Issue
- U.S. Centers for Disease Control and Prevention’s Division of STD Prevention
- USA & Canada
- Yale School of Public Health
- Yonatan H. Grad







No comments yet