A study reported in Proceedings of the National Academy of Sciences (PNAS) shows how the presence of a specific protein called IL-22BP affects the composition of the gut microbiota and the body’s response to bacterial infection.
“We discovered that mice that don’t produce this protein are more protected against intestinal infections by bacteria like Clostridioides difficile and Citrobacter rodentium,” Marco Aurélio Ramirez Vinolo, a co-author of the article, said. He is a professor at the State University of Campinas’s Institute of Biology (IB-UNICAMP) in Brazil and head of its Immunoinflammation Laboratory.
READ MORE: Key role found for gut epithelial cells in the defense against deadly diarrheal infections
READ MORE: Violin resin effective against deadly pathogens - even in dirty conditions
IL-22BP (interleukin 22 binding protein) reduces the available amount of IL-22, a protein produced by immune system cells that helps maintain the intestinal barrier, strengthens gut lining cells, and is involved in the production of antimicrobial substances.
Strengthening intestinal defenses
“Our explanation for this finding is that interleukin 22 is more effective in the absence of IL-22BP, in terms of strengthening the intestinal defenses even before an infection begins,” said Vinolo, who received funding from FAPESP for a study of the molecular mechanisms involved in gut microbiota during inflammation.
In the PNAS article, the researchers report that the mice without IL-22BP had different gut bacteria and that when these bacteria were transferred to the mice with normal production of IL-22BP, they were nevertheless protected against infection, suggesting that the absence of the binding protein resulted in beneficial modulation of the gut microbiota.
“This resistance to infection was associated with increased production of short-chain fatty acids, which are released by the fermentation of food fiber by gut bacteria and have beneficial effects on intestinal health, including promotion of an anti-inflammatory environment and strengthening of the intestinal barrier,” said José Luís Fachi, first author of the article and a postdoctoral fellow at Washington University School of Medicine (WUSM) in the United States.
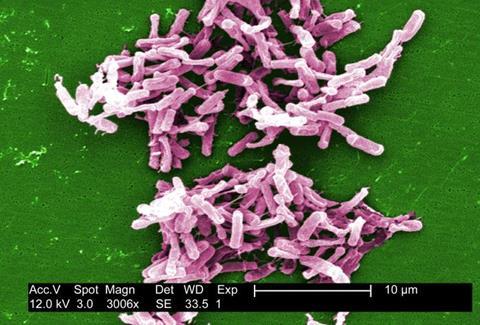
Gut bacteria
Fachi was supported by FAPESP during his PhD research on the interaction between gut bacteria and colonization by C. difficile, a bacillus resistant to several antimicrobial agents and a frequent cause of hospital-acquired infections. Short-chain fatty acids are produced by the bacterial metabolism during the fermentation of food fibers and protect the gut from infections such as those caused by C. difficile.
The absence of IL-22BP modifies the composition and functionality of gut microbiota, resulting in a beneficial profile for the organism, according to Vinolo, who was Fachi’s doctoral thesis advisor. “This highlights the role of gut microbiota in regulating the organism’s responses and points to the possibility of attenuating or preventing intestinal infections via IL-22BP inhibition,” he said.
Next steps
Future studies can now be designed to understand the discovery in greater depth and use it to develop treatments. “The essential next step is to investigate the efficacy of IL-22BP inhibitors in animal models and possibly in clinical trials to treat severe intestinal infections,” Fachi said. Another possibility will be to explore how different types and quantities of food fiber affect short-chain fatty acid production. “The composition of gut microbiota in the absence of IL-22BP can provide valuable information,” he added.
Gut microbiota modulation may benefit other intestinal inflammatory conditions, such as Crohn’s disease and ulcerative colitis, as well as infections caused by other pathogens.
“Finding out how IL-22 interacts with other molecules and immune system cells in the absence of IL-22BP will help us better understand its function in intestinal immunity. Future studies could transform our understanding of the role of these proteins in intestinal health and lead to the development of novel therapeutic strategies to prevent and treat intestinal infections,” Vinolo said.
The study involved researchers in IB-UNICAMP’s Department of Genetics, Evolution, Microbiology and Immunology, and WUSM’s Department of Pathology and Immunology.







No comments yet