The pathogenic fungus Aspergillus fumigatus escapes elimination from surface cells of the human lung by binding to a human protein. In doing so, it is able to nest in so called phagosomes, confined areas in the lung cells, and thus prevents cell processes that would kill the fungus from being set in motion.
Researchers at the Leibniz Institute for Natural Product Research and Infection Biology (Leibniz-HKI) have thus discovered a possible new target against the fungal infection.
Aspergillus fumigatus is an environmentally prevalent mould found worldwide. For people with a weakened immune system, it can become a serious threat: according to estimates, yearly more than 300,000 people worldwide contract invasive aspergillosis, an infection with a mould of the genus Aspergillus. An estimated 40-90 percent of the patients die from it.
Surface cells
Researchers at Leibniz-HKI have now discovered that fungal spores can inhibit the protective response of surface cells of the lungs.
“These epithelial cells in our lungs are an important barrier against fungal spores and other potential pathogens in the air,” explains Axel Brakhage, director of the Leibniz-HKI and professor at Friedrich Schiller University in Jena. They keep out a large portion of the spores we breathe in every day.
Unlike immune cells, lung epithelial cells are not specialised in killing pathogens, but are nevertheless capable of doing so: the cells enclose foreign bodies to form a membrane-confined compartment known as a phagosome. Subsequently, a multitude of cellular processes is set in motion, during which the phagosome matures and the intruders are dissolved by highly reactive substances.
The researchers discovered that fungal spores can redirect this mechanism when they took a close look at their surface structures.
“We wanted to know which of the fungal surface proteins could bind to human cells and thus be involved in the infection,” explains Leijie Jia, lead author of the study.
Hijacking protein
They found that the human protein p11 appears to be bound by a fungal protein.
“When we switch off the fungal protein that binds to p11, we find the fungal spores in the ‘mature’ phagosomes, which means they are killed. If we knock out the human p11, likewise,” says Jia. “However, if the fungal protein and p11 are intact, the phagosomes remain ‘immature’.”
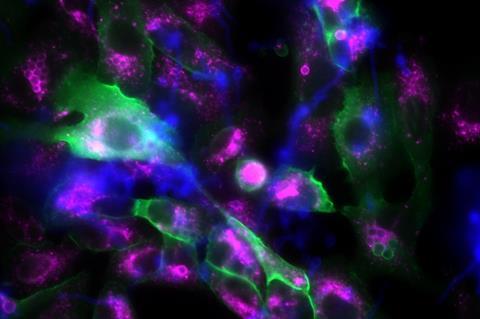
Then the epithelial cells of the lung contain the fungal spores but do not destroy them. Jia and his colleagues at Leibniz-HKI were also able to observe this phenomenon under the microscope; the spores germinated in the immature phagosomes and formed fungal hyphae. Some of the spores were also released out of the cell again or transferred into a neighbouring cell so that the fungus could spread.
The researchers were also able to repeat the experiments with immune cells. This means that the fungal spores can not only hijack phagosomes in the lung cells, but also in various immune cells.
Transplant implications
The clinical significance of their discovery was further investigated by the team from Jena together with medical scientists from Portugal, who provided DNA data from recipients and donors of a stem cell transplant.
“After transplantation, patients are particularly susceptible to fungal infections because the immune system is shut down,” explains Axel Brakhage. A good quarter of the approximately 500 stem cell transplant recipients who took part in this study developed life-threatening invasive aspergillosis in the months after the transplant.
Promisingly, the researchers discovered an important clue when comparing the genetic analysis with disease outcome.
“Patients with a particular mutation in the p11 gene were less likely to develop invasive aspergillosis. This result helps to keep a particularly close eye on patients who are more at risk,” says Jia. Both the fungal protein that binds to p11 and the human protein itself are possible targets for treatment of the fungal infection.
The work was funded by the Deutsche Forschungsgemeinschaft (German Research Foundation, DFG) within the framework of the Balance of the Microverse Cluster of Excellence and the Collaborative Research Centres FungiNet (Transregio) and PolyTarget, among others. The work received further support from the Leibniz Association, the Fundação para a Ciência e a Tecnologia, the EU within the framework of Horizon 2020, the “la Caixa” Foundation and the Gilead Research Scholars Program.







No comments yet