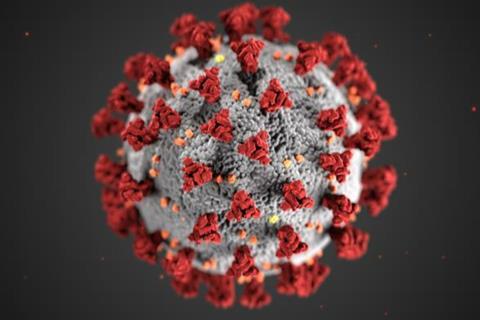
A new study finds differences in gut bacteria and metabolites among COVID-19 patients admitted to the ICU, offering possibilities for preventing the worst outcomes.
In early 2020, Bhakti Patel, MD, a pulmonary and critical care specialist at the University of Chicago Medicine, and Matthew Stutz, MD, came up with the idea of studying the gut microbiome of patients admitted to the ICU to see if it could help them understand why some patients recover and do well after discharge from the hospital, and others continue to suffer from debilitating complications.
“We were trying to tie together factors that might lend itself to a biologic explanation of why patients get disabled after surviving an ICU stay that goes beyond just the stuff that we do that could have complications,” said Patel, who is an Assistant Professor of Medicine.
During the Covid outbreak, Patel worked on an innovative, helmet-based ventilation system that helps prevent critically ill patients from being put on a ventilator. Meanwhile, she and Stutz, who now works at Stroger Hospital in Chicago, pivoted their project to an opportunity to understand the role of the microbiome in severe COVID-19 infections.
The results of this work, published in Nature Communications, show that the composition of gut microbiota and the metabolites they produce can predict the trajectory of respiratory function and death in patients with severe COVID-19. This suggests that the gut microbiome has important links to lung health and presents an opportunity to prevent the worst outcomes.
Divergent outcomes
Patel said one of the most troubling things during the pandemic was seeing patients who were relatively healthy come into the ICU and have completely different outcomes. Some died, some ultimately recovered, and many recovered but were left with lasting complications.
“This tells me there is something else going on, and this study shows that there was some interaction between their microbiome health and how they recovered from their infection.”
Between September 2020 and May 2021, nurses collected faecal samples from 71 patients with COVID-19 as they were admitted to the medical ICU at UChicago Medicine; 39 of these patients survived, and 32 later died.
To analyze the samples, the physicians turned to scientists at UChicago’s Duchossois Family Institute(DFI), who have extensive, on campus expertise and technical infrastructure to study the composition of the microbial samples, including the metabolites and other chemical compounds that microorganisms in the gut consume and produce.
Critical timing
Eric Pamer, MD, the Donald F. Steiner Professor of Medicine and Director of the DFI, said the careful timing of sample collection is critical, because it enabled Stutz and Patel to make meaningful comparisons between patients who were admitted with similar severities of COVID-19, but went on to either recover from infection or develop progressive respiratory failure. This allowed them to ask whether progression of infection is impacted by the microbiome and the metabolites it produces, specifically in an ICU setting.
“It can be very informative to to investigate groups of patients with similar infections that inexplicably follow different clinical courses, either improving or becoming increasingly compromised” he said. “The study led by the Pulmonary Critical Care team gave us an opportunity to see if there were differences in the microbiomes of patients who recovered or worsened.”
Microbiome differences
The DFI’s core facilities detected several notable differences in the composition of the microbiome and metabolic products among these patients. Patients who suffered progressive lung failure and died had more of a group of bacteria called Proteobacteria than patients who recovered. These patients also had lower levels of secondary bile acids, and less of a metabolite called desaminotyrosine. Conversely, the patients who improved had higher levels of secondary bile acids and more desaminotyrosine.
Pamer said these findings are exciting because preliminary research has shown that secondary bile acids help moderate immune responses, and desaminotyrosine has been linked to improved antiviral immune defenses. But it raises a chicken versus egg question: Did the patients who survived come into the ICU with a protective microbiome, or did the severe infection damage the microbiome of those to who died?
It’s still too early to tell, but Pamer says the meticulous timing of sample collection in this study revealed differences in patients prior to deterioration or recovery, suggesting that the microbiome and the metabolites contribute to recovery from severe respiratory infection. That could open a window for giving patients probiotic treatments containing the right strains of bacteria to produce protective metabolites.
Analyzing their microbiome could also identify patients likely to develop progressive disease, giving clinicians a chance to intervene preemptively. The DFI is currently building a facility certified for producing such treatments, such as capsules that include live bacteria that can help reconstitute a patient’s microbiome.
A systems-based intervention
Patel said having a resource like the DFI on campus is a boon to her work trying to create the best possible outcomes for patients leaving the ICU. “As a bedside provider, I can already tell if a patient is in bad shape. I don’t necessarily need a stool sample for that,” she said. “But what it does is allow me to ask a lot more questions, like how frail is this patient given all the medical problems they came in with? How is that going to interact with the infection they have now? And how can we supplement the microbiome to build up that resilience to avoid, for example, going on a ventilator?”
“That’s the exciting thing about collaborating with the DFI team,” she continued. “This discovery about metabolite production and its interaction with the immune response represents a paradigm shift in microbiome research. With the technology provided by the DFI, we can measure the microbiome function within hours and leverage that lead time to customize interventions where we can restore someone to a healthier state. I think this is just the beginning of many stories we can tell together.”






No comments yet