Our bodies have always known how to fight infectious microbes; even new, emerging, and more dangerous ones that threaten our health. This is achieved via specific immunity, which occasionally needs a helping hand to make it more timely and effective. Indonesia has its own particular microbial and immunological landscape, which new collaborative projects aim to better define and address through monitoring, vaccination, and concerted regional endeavors.
Infectious diseases (IDs) are a major health issue in Indonesia, as in many tropical low- and middle-income countries (LMICs), placing a significant economic burden on limited resources. These concerning IDs comprise a wide range of viruses, bacteria, and parasites that cause variable degrees of morbidity and mortality.
Countries such as Indonesia are a hotbed for the emergence of antibiotic resistance and new pathogenic varieties of microbes, due partly to a dense, low socio-economic population living in close proximity to domesticated animals. In addition, the consistently hot and humid climate enables the rapid spread of pathogens via the environment and by vectors such as mosquitos. Indonesia is a large country in terms of population (280 million) and sheer size; comprising 14,000 islands and being over 5000 kilometers in length, creating great challenges for the country’s Ministry of Health (MoH) in managing IDs.

International collaboration
Advances are being made to improve the understanding of the microbial landscape in Indonesia through collaborations with the Centers for Disease Control and Prevention (CDC), the United States Agency for International Development (USAID), and World Health Organization (WHO). Together with other organizations and institutions, this is strengthening Indonesia’s preparedness and resilience to emerging threats in the aftermath of the COVID-19 pandemic. The recommendations from such bodies are translated into action, such as through the Severe Acute Respiratory Infections (SARI) and Influenza-Like Illness (ILI) sentinel surveillance programs, as well as their associated Emerging Infectious Diseases (EID) risk mapping. This activity links with the collection and curation of microbial isolates from infected individuals, with patient demographics and clinical features, and the microbial characterization for properties such as antibiotic resistance, DNA sequence variation, and ability to be neutralized by antibodies.
With the Field Epidemiology Training Program (FETP), WHO and MoH have conducted training for 15 SARI sentinel hospitals and 26 ILI sentinel primary healthcare centers. The sentinels are crucial for identifying new infectious diseases early, as they monitor symptoms similar to those of flu and severe respiratory infections, providing a real-time early warning system for potential outbreaks before they spread widely. Since over 60% of EIDs affecting humans have animal origins (zoonoses), a holistic One Health approach has been established that considers the interconnectedness of human, animal, and environmental factors. Leading the One Health Initiative, the Quadripartite Organizations – WHO, the UN Food and Agriculture Organization (FAO), the World Organization for Animal Health (WOAH), and the UN Environment Programme (UNEP) – jointly developed the One Health Joint Action Plan of Action (OH JPA). This provides a solid foundation for action, with a focus on enhancing collaboration, communication, capacity building, and coordination across all sectors to fortify health security.

Microbes and immunity
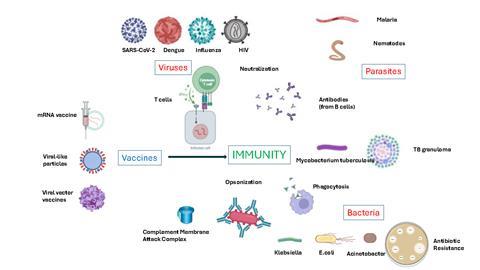
Another key element of this microbial-related landscape is immunity to ID microbes, which may be generated by natural exposure to, or infection with the organisms, or by immunization through specific vaccines. Such immunity is referred to as “adaptive” immunity since it is generated through the “education” of T cells and B cells which specifically respond to elements of the microbe called antigens. B cells produce antibodies specific to the microbial antigens which can inhibit the microbe in a number of ways.
Neutralizing antibodies bind to key molecules of microbes disabling their ability to bind and infect human host target cells (as in anti-Spike antibodies in SARS-CoV-2 infection), or their ability to create toxicity in the human host (as in Diphtheria). Antibodies may help to clump bacteria to facilitate their improved clearance from moist mucosal surfaces of the body (pneumococci in the lungs). Antibodies can also label (opsonize) their microbial targets, flagging them to be attacked by destructive complement proteins or to be “eaten” by phagocytes (macrophages and neutrophils). T cells, particularly cytotoxic T lymphocytes (CTL) expressing the CD8 marker, are effective at detecting human host cells harboring certain microbes and thus eliminating the cells and the microbes within them. Helper T cells, expressing CD4, orchestrate all adaptive immune responses, including antibody production by B cells and CTL activity, and also cause the hyperactivation of macrophages to facilitate bacterial destruction, particularly mycobacteria. The concept of “herd immunity”, where a broadly immune population can prevent infection of those without immunity, is particularly important and useful and requires immune monitoring to establish if it exists.
Such efforts at immune monitoring are underway in Surabaya, with an initial focus on SARS-CoV-2, which will expand into other key viruses, bacteria, and parasites. New variants will be identified through sequencing, and variants of Spike antigen will be produced as recombinant proteins and tested for antibody recognition and cross-reaction with other variants.
Major threats and the response in Indonesia
Across the tropical LMICs, the “big three” IDs – malaria, tuberculosis, and HIV – remain major challenges and are targets for new or improved vaccines. However, the recent COVID-19 pandemic has starkly highlighted the potential threats from emerging IDs, particularly those of the respiratory tract and where no pre-existing immunity exists. The key viral infections in Indonesia are thus SARS-CoV-2, dengue, influenza, Human Immunodeficiency Virus, viral hepatitis, and Human papillomavirus. For bacterial infections, the full widespread uptake of existing vaccines in key groups is a challenge that the Indonesian MoH is embracing. Examples of this are vaccines against pneumococcus and meningitis in infants and the elderly.
There are several less well-publicised, yet nonetheless important bacterial species being observed in Surabaya for their incidence and antimicrobial resistance (AMR). These are Enterobacteriaceae species including Klebsiella pneumoniae, Escherichia coli, and Salmonella spp., as well as non-lactose fermenting pathogens such as Acinetobacter baumanii, which possess resistance to key antibiotics, particularly via producing extended-spectrum beta-lactamase (ESBL) and carbapenemase. Multi-drug resistance is a particular issue. These are often hospital-acquired infections and pose a unique challenge to the MoH. A decades-long epidemic of bacterial infections untreatable by first-line medicines is exacerbated by patient noncompliance with treatment recommendations, over-prescription, and misuse. Commercially available antimicrobials are thus becoming ineffective due to the global increase in antimicrobial resistance. It is as yet unclear whether treatment of these IDs would benefit from the use of vaccines, but it is the subject of our current work.

A role for vaccines?
Ensuring vaccine security and self-reliance is an essential priority for all nations if they are to escape the worst health and economic impacts of future pandemics. For LMICs, this is best achieved with a wider regional approach. Existing geopolitical and economic alliances and a strong baseline of biopharmaceutical manufacturing mean that Southeast Asia is well-positioned to become a global leader in vaccine production. The newly launched UK-South East Asia Vaccine Manufacturing Research Hub will support this ambition by addressing key priorities, including technology transfer, intellectual property, standardization, and supply chain. The Hub is currently focussing on Dengue, Hand Foot and Mouth Disease virus, TB, Rabies, and viral hepatitis. The main vaccine platforms are mRNA, recombinant proteins in virus-like particles, and viral vectors such as adeno-associated virus. As highlighted in the One Health initiative, transmission of infectious diseases from animals is a major focus, and vaccines for animals are being investigated.
Vaccination may have a critical role to play in the prevention of zoonotic infectious diseases. The goal of vaccination is nearly always the directly affected animal species, and there are not many schemes for how this could be done in practice, to prevent human disease indirectly. Since biopharmaceutical industry divisions for human and animal health are typically segregated, emphasis could be placed on vaccine-based strategies that combine veterinary and human medicine as integrative preventive measures.
A multi-faceted approach to managing IDs in Indonesia, comprising microbiological and immune monitoring, and tailored local vaccine design and manufacture, will greatly benefit Indonesia’s countrywide and regional health and prosperity over the coming years, strengthening preparedness and resilience to emerging threats.








No comments yet