New research published in the journal Proceedings of the National Academy of Sciences sheds light on the pathways that drive organ damage and death in severe COVID-19 and helps explain why survivors of the disease can experience long-term complications.
“Our study resolves some of the long-standing unanswered questions about how the SARS-CoV-2 virus impacts the body,” said co-senior author Afshin Beheshti, Ph.D., professor of surgery and computational and systems biology at the University of Pittsburgh School of Medicine and associate director of the McGowan Institute for Regenerative Medicine. “The findings point to new avenues for developing therapies to prevent or mitigate severe COVID-19 outcomes and possibly reduce the risk of long COVID.”
For the study, Beheshti, who is president of the COVID-19 International Research Team (COV-IRT), brought together a multi-institutional group, including researchers from Johns Hopkins University, Children’s Hospital of Philadelphia (CHOP) and Weill Cornell Medicine.
Cytokine storm
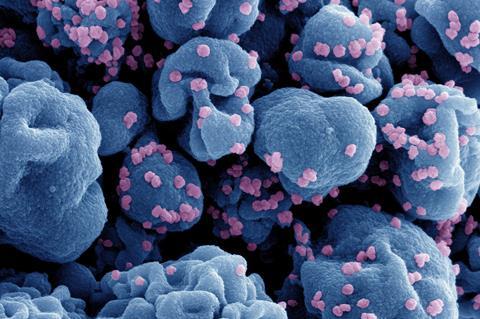
By analyzing the expression of genes in nasal swab samples from patients with severe COVID-19 compared to those from healthy people, the researchers found that SARS-CoV-2 disrupts essential reactions in the mitochondria, the cell’s energy-producing factories. Mitochondrial stress led to the release of compounds that act as danger signals, which in turn trigger immune sensors that activate the renin-angiotensin-aldosterone system (RAAS).
READ MORE: New therapeutic approach for severe COVID-19
READ MORE: Zoonotic transmission of Covid has led to infections in more than 30 mammalian species
RAAS is a network of hormones, proteins and enzymes that is essential for regulating blood pressure but can trigger a cascade of organ-damaging events when overactivated. In severe COVID-19, overactivation of RAAS and mitochondrial stress intensifies an out-of-control immune reaction called a “cytokine storm” often seen in patients with severe COVID-19.
Unique among COVID-19 studies, this research used a comprehensive analysis of autopsy samples to analyze organs of patients who died from the disease. They found that overactivation of RAAS and a cytokine storm combined to create a hurricane of inflammation that wreaked havoc in multiple organ systems, leading to heart failure, myocardial injury in the heart, pulmonary fibrosis and chronic kidney disease, all conditions often seen in long COVID patients.
Substantial damage to the lymph nodes
“Notably, we also found that activation of RAAS caused substantial damage to the lymph nodes, which hasn’t been shown in COVID-19 before,” said Beheshti, who is also director of McGowan’s Center for Space Biomedicine. “This could explain the long-lasting immune dysregulation seen in survivors of COVID-19 and may contribute to long COVID.”
It’s also possible that damage to lymph nodes could impair the immune system’s ability to detect and destroy cancerous cells, which could potentially help explain the post-pandemic increase in cancer cases.
According to Beheshti, the new findings suggest that targeting RAAS overactivation and supporting mitochondrial function could be new approaches for developing therapeutics to prevent or mitigate severe COVID-19 outcomes and potentially reduce the risk of long COVID.







No comments yet