A new study from Uganda provides the first evidence to date that resistance to a lifesaving malaria drug may be emerging in the group of patients that accounts for most of the world’s malaria deaths: young African children suffering from serious infections.
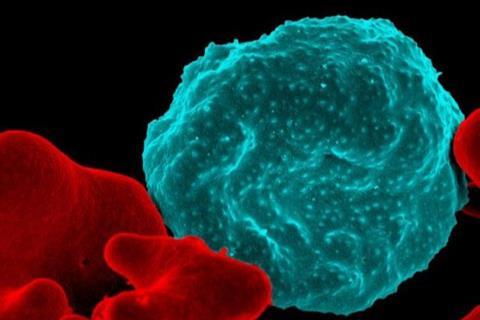
The study, presented at the Annual Meeting of the American Society of Tropical Medicine and Hygiene and published in the Journal of the American Medical Association (JAMA), documented partial resistance to the malaria drug artemisinin in 11 of 100 children, ages 6 months to 12 years, who were being treated for “complicated” malaria, that is, malaria with signs of severe disease caused by the malaria parasite Plasmodium falciparum.
READ MORE: Scientists design new drug to fight malaria
READ MORE: New agent effective against drug-resistant malaria parasites
Also, 10 patients who were thought to have been cured suffered a repeat malaria attack within 28 days from the same strain of malaria that caused the original infection, suggesting that the initial treatment did not fully kill the infecting parasites.
First study from Africa showing partial resistance to artemisinin
“This is the first study from Africa showing that children with malaria and clear signs of severe disease are experiencing at least partial resistance to artemisinin,” said Chandy John, MD, MS, director of the Indiana University School of Medicine Ryan White Center for Infectious Diseases and Global Health, who is a co-author of the study along with colleagues Ruth Namazzi and Robert Opoka from Makerere University in Kampala, Uganda. John, who is a former ASTMH president said, “It’s also the first study showing a high rate of African children with severe malaria experiencing a subsequent malaria episode with the same strain within 28 days of standard treatment with artesunate, a derivative of artemisinin, and an artemisinin combination therapy (ACT).”
The arrival of artemisinin therapies some 20 years ago was a major advance in the global fight against malaria due to their power to rapidly cure infections — and because malaria parasites had developed resistance to other drugs. In 2008, there were reports from Cambodia noting partial resistance to artemisinin. By 2013 there was evidence that in some patients, the drug was completely failing. In the last few years, there has been increasing evidence that artemisinin resistance has now spread from that region into East Africa. The prospect of artemisinin losing its efficacy is particularly alarming for Africa and especially for African children. The region accounts for 95% of the 608,000 people who die from malaria each year and a large majority of malaria deaths in Africa are children under 5.
Malaria parasites with genetic mutations
While all of the children in the study eventually recovered, 10 of them were infected with malaria parasites that harbor genetic mutations that have been linked to artemisinin-resistance in Southeast Asia. The study noted that while these mutations have been documented in Africa in less severe cases, this was the first time they have been seen in parasites that were causing complicated malaria in hospitalized African children. The term “complicated” malaria is used to define cases where the disease is at risk of causing potentially life-threatening complications, like severe anemia or brain-related problems known as cerebral malaria.
John said that researchers classified patients as suffering from partial resistance based on the World Health Organization’s defined half-life cutoff for parasite clearance of more than five hours, meaning requiring more than five hours to reduce a patient’s parasite burden by 50%. Two children required longer than the standard maximum of three days of artesunate therapy because they failed to clear their parasites with three days of therapy. He said longer treatment times increase the risk of poor outcomes. Also, he said that in Southeast Asia, the path to broadly resistant malaria parasites started with evidence of partial artemisinin resistance, and the concern is that pattern will be repeated in sub-Saharan Africa.
High number of recurrent cases
The Ugandan children in the study received what is considered to be the gold standard for treating complicated malaria infections: an intravenous infusion of artesunate followed by oral treatment with an ACT that combines another derivative of artemisinin, a drug called artemether, with the malaria drug lumefantrine.
John said the relatively high number of recurrent cases raises concerns that the efficacy of lumefantrine also may be declining. The drug is paired with artemether to make it harder for parasites to develop artemisinin resistance and also because lumefantrine stays in the body longer than artemether. Therefore, it can kill any remaining parasites not cleared by the shorter-acting artemisinin.
John said the study emerged from ongoing work in Uganda that is investigating outcomes of children who experience episodes of severe malaria. He said researchers pivoted to a focus on drug resistance because they noticed some children appeared to be slower to respond to the infusion of artesunate followed by an oral ACT.
“The fact that we started seeing evidence of drug resistance before we even started specifically looking for it is a troubling sign,” John said. “We were further surprised that, after we turned our focus to resistance, we also ended up finding patients who had recurrence after we thought they had been cured.”
Topics
- Antimicrobial Resistance
- artemisinin
- artemisinin combination therapy
- artemisinin-resistance
- Chandy John
- Indiana University School of Medicine
- Infectious Disease
- Makerere University
- malaria
- Middle East & Africa
- One Health
- Parasites
- Plasmodium falciparum
- Research News
- Robert Opoka
- Ruth Namazzi
- Ryan White Center for Infectious Diseases and Global Health
- USA & Canada







No comments yet