A study has compared the development of HIV reservoirs – locations in the body where the virus persists in a latent state – between patients who receive either early or late medical interventions. The findings highlight the importance of timely treatments for managing the virus.
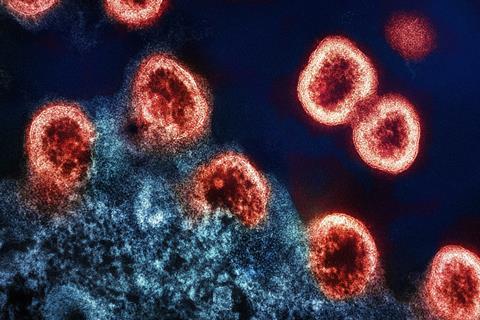
The research, published today as a Reviewed Preprint in eLife, is described as important and timely by the eLife editors. They particularly praise the study’s focus on the subtype C variant of HIV’s effect on women from southern Africa, which are both significantly understudied in the field. The strength of evidence, described as convincing, supports the conclusion that, although early treatment does not prevent the formation of HIV reservoirs, it is associated with a faster decay of virus reservoirs.
The results indicate that, when combined with other interventional strategies, early treatment with antiretroviral therapy (ART) could enable an eventual cure for HIV.
Immune system
HIV attacks the body’s immune system, weakening it over time and leaving the body less able to fight off infections and certain cancers. Studies show that a person living with HIV has a similar life expectancy to an HIV-negative person – provided they are diagnosed in good time, have good access to medical care, and are able to adhere to their HIV treatment.
However, treatment, which usually involves ART, is lifelong as it cannot eradicate the virus hiding in reservoirs. This may be financially unsustainable in lower-income countries, which are often more affected by the HIV epidemic. People living with HIV may also be at higher risk for other comorbidities because their immune systems appear to remain suboptimal even when they are on antiretroviral therapy.
“Designing globally applicable HIV interventions, or eventually a cure, requires a much deeper understanding of the nature of HIV reservoirs: their variability in size, composition and genetic characteristics,” says lead author Kavidha Reddy, a research associate at the Africa Health Research Institute, KwaZulu-Natal, South Africa. “Reservoir studies in subtype C HIV infections are limited, despite it being the most prevalent form globally and predominating in southern Africa. Moreover, data are lacking in women, despite known sex differences in immune responses to HIV infections.”
Rapid viral replication
To remedy this, Reddy and colleagues recruited 35 women from Durban, South Africa, to participate in the study. The cohort was split into two groups: early-treated, who began ART a day or two after detection of acute viremia, and late-treated, who began treatment over a year after detection of viremia. The cohort was unique because all the women were followed up and tested regularly for HIV from when they were HIV negative, allowing the researchers to detect acute HIV infection. This refers to the earliest stages of infection, where rapid viral replication occurs in the body.
To gain insights into the nature of HIV reservoirs in the two groups, the team first measured the total amount of HIV DNA present in blood cells at baseline (one to three days after detection of HIV), peak viremia, and after 6–12 months of ART, using a technique called droplet digital polymerase chain reaction (ddPCR). At baseline, HIV DNA was detectable in both groups. At peak viremia, HIV DNA levels in the early-treated group were even comparable to that which would be expected in someone who receives no treatment at all.
Over a year of ART, the team observed a steady decline in HIV DNA in the early-treated group that was not seen in the late-treated group – however, this decline was not sufficient to eradicate the virus in a realistic timeframe. These observations confirmed previous reports that HIV reservoirs are formed during the earliest stages of infection, possibly before the virus can be detected free in the blood – that is, before viremia.
HIV reservoirs
Next, the team assessed whether the HIV detected within immune cells (the reservoir) has the potential to replicate, using a next-generation sequencing technique called FLIP-seq. HIV that is able to replicate within cells is genome-intact, and, if it cannot, it is genome-defective.
In both groups, genome-intact cells could be detected before treatment initiation. In the late-treated group, genome-intact cell numbers decreased after one year of ART, but remained present. In contrast, in the early-treated group, genome-intact virus numbers decreased rapidly after ART initiation, such that they were no longer detectable after one year of treatment.
The team caution that they cannot rule out that sampling more cells in blood or tissues would detect genome-intact HIV in this group. Nevertheless, these findings strongly suggest that early treatment initiation facilitates a faster clearance of HIV cells that have the potential to reignite virus replication if antiretroviral therapy was stopped.
Genome-intact HIV cells
In addition, the team observed that genome-intact HIV cells decayed faster than genome-defective cells in both treatment groups. This is possibly because cells containing intact genomes are preferentially targeted by the immune system.
Early treatment resulted in a faster decay of both genome-intact and genome-defective HIV cells, suggesting a more effective immune clearance mechanism in this group permitted by early ART, and further highlighting the importance of early interventions to combat HIV.
“To our knowledge this is the first study in an African population that examines the impact of the timing of ART initiation on HIV subtype C reservoirs,” says Reddy. “Most studies have focused on men with subtype B infections – which is more prevalent in Western countries. Yet young women carry the heaviest HIV burden in sub-Saharan Africa, where subtype C dominates and comprises nearly 50% of HIV infections globally. Therefore it was important for us to investigate how the subtype C virus affects women in particular, as it cannot be assumed that any interventions would perform the same in men and women or across different populations.”
Rapid decay
“Overall, our results confirm previous reports that early interventions with ART do not prevent the formation of reservoirs. However, we show that early treatment is associated with a more rapid decay of genome-intact HIV, a decrease of genetic complexity across the reservoir, and prevents escape from the immune system,” concludes senior author Thumbi Ndung’u, Director for Basic & Translational Science at the Africa Health Research Institute.
“Our results highlight the importance of early treatment to combat HIV, and suggest that when combined with other interventional strategies, it is more likely to enable an eventual HIV cure.”






No comments yet