The opportunistic bacterial pathogen Pseudomonas aeruginosa is dangerous due to its resistance to multiple antibiotics. A research team from Heinrich Heine University Düsseldorf (HHU) and Jülich Research Center (Forschungszentrum Jülich – FZJ) has now found a mechanism that makes it possible to weaken the virulence of the pathogen. Based on this knowledge, a new approach for antibiotics can be developed, as the authors explain in the scientific journal JACS Au.
The bacterium Pseudomonas aeruginosa often causes a so-called “nosocomial infection” in humans. It is therefore one of the dangerous hospital bacteria that is resistant to several antibiotics. Immunocompromised patients are particularly affected. The World Health Organisation (WHO) has placed P. aeruginosa on the list of “priority pathogens” on which research efforts should focus to find new treatment options.
Virulence factors
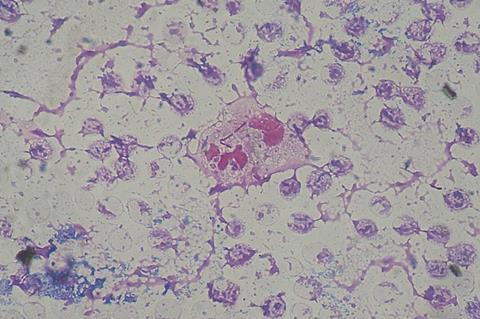
The bacterium has a broad spectrum of disease-causing virulence factors. These include the “type A phospholipases” (PLA1): Enzymes that can damage the membrane of the host cell and also disrupt various signalling networks in the infected cells. Preliminary work (DOI: 10.7554/eLife.72824) has shown that the enzyme PlaF from P. aeruginosa is a PLA1 that also alters the membrane profile and thus contributes to the virulence of the bacterium.
The research groups of Professor Dr Holger Gohlke (HHU Institute of Pharmaceutical and Medicinal Chemistry and IBG-4: Bioinformatics at FZJ) and Professor Dr Karl-Erich Jaeger (HHU Institute of Molecular Enzyme Technology at FZJ) have now identified molecular mechanisms in which medium-chain free fatty acids regulate the activity of PlaF.
The researchers carried out molecular simulations as well as laboratory studies and in vivo assays. All of these research approaches showed an indirect effect of the fatty acids on the location of PlaF in the bacterial membrane as well as a direct effect by blocking the active centre of the enzyme. In both ways, the activity of PlaF is reduced.
Complex relationships
On the one hand, the results provide evidence that the interplay of mechanisms is a regulatory factor for PlaF function. Professor Gohlke says: “We were only able to unravel these complex relationships through the interaction of computer-aided and experimental techniques within the framework of the projects funded by the CRC 1208.”
On the other hand, the results contribute to understanding the regulatory role of fatty acids. It may be possible to transfer the results to other membrane proteins that have a similar structure to PlaF.
Finally, they also open up new perspectives on how PlaF can be inhibited. Professor Jaeger says: “This is a promising approach for developing new antibiotics against P. aeruginosa. These are urgently needed to combat the dangerous pathogens in hospitals.”






No comments yet