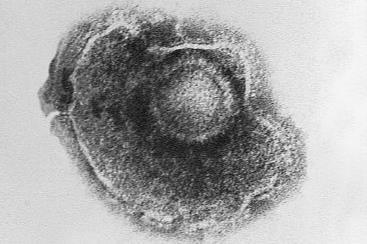
Scientists at the University of Colorado Anschutz Medical Campus have discovered a new evasion strategy used by the varicella zoster virus, which causes chickenpox and shingles, that may allow it to affect tissues far from the original site of infection.
The study was published in the Journal of Virology.
READ MORE: Live shingles vaccine still protecting 10 years on - despite waning effectiveness
READ MORE: Has a viral contribution to Alzheimer’s disease been in front of our noses this whole time?
The researchers, using human neurons and rodent models, honed in on a single viral protein known as IE62 that is packaged and shuttled throughout the body in structures known as small extracellular vesicles (sEVs). They discovered that IE62 packaged inside sEVs can travel from the site of infection, where it penetrates cells and shuts down their antiviral response, opening the door to infection by the virus.
Ancient and common
The virus, known as VZV, is ancient and common, residing within 95% of all people. Its primary infection causes chickenpox, which then goes latent. During stress, aging, or other factors, VZV can reactivate into shingles, a painful skin disease that can also attack the central nervous system and can lead to vascular disease, stroke, dementia, and other serious conditions.
To rapidly spread throughout the body, the virus needs an immediate strategy to evade the immune system. This study is the first to show exactly how it does this by exploiting the infected cells sEV machinery.
“This is the first time a clear mechanism has been found that actually ties this virus to an avenue by which it can affect distal organs, far from the site of infection,” said the study’s first author, Christy Niemeyer, PhD, assistant professor of neurology at the University of Colorado School of Medicine. “These vesicles shut down the immune response.”
Important protein
The study’s senior author Andrew Bubak, PhD, assistant professor of neurology at the CU School of Medicine, said the protein shuts down the anti-viral response in the cells far sooner than previously known.
“We believe this protein is likely being packaged into sEVs and shuttled down the neurons that go to your skin, making the cells under the skin vulnerable to the whole infection,” Bubak said. “We think this precedes the rash, which is obviously interesting from a therapeutic standpoint.”
While there is a vaccine for shingles, there are currently no drugs to impact the activity of this protein. That could change.
“This study is the first to identify a different anti-viral target that perhaps we can develop therapeutics for,” Niemeyer said.
Prevalent co-infections
Bubak said this mechanism may be responsible for the prevalent co-infections and immunosuppressive events seen clinically in those infected with VZV. He also noted that the virus can intermittently reactivate in individuals without the classic shingles rash, evading diagnosis and raising the question of whether this immunosuppressive event occurs more frequently than originally thought.
“This mechanism can offer us clues into how other viruses work and cause infection,” he said.
Niemeyer agreed, saying the significance of sEVs in the spread of this virus highlights the need for further investigation.
“We need to better understand their role in viral spread and secondary disease development to reduce the systemic complications caused by VZV infections,” she said.







No comments yet