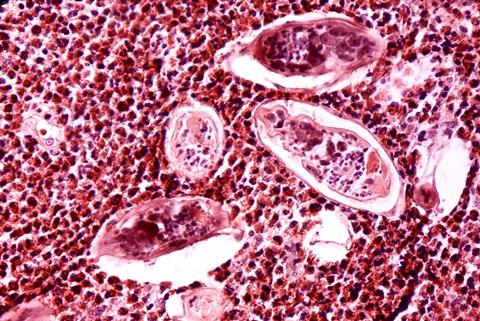
Schistosomiasis is a widespread parasitic disease, particularly prevalent in regions with poor access to clean water and sanitation.2
READ MORE: Probe into human cervical stem cells shows lactic acid bacteria can prevent cervical cancer
READ MORE: Street science brings home an important message about African sleeping sickness
S. haematobium, one of the main species responsible for human schistosomiasis, infects over 110 million people worldwide by depositing eggs that infiltrate the urinary and reproductive tracts.3 While this parasite is recognised as a cause of bladder cancer, its potential role in cervical cancer has remained poorly understood.
Cervical tissue
In this study, researchers analysed cervical tissue samples from 39 Tanzanian women with (n=20) and without (n=19) S. haematobium infection. Infected women received praziquantel treatment, and samples were collected at baseline and 4-12 months post-treatment.
Through RNA sequencing and gene expression analysis, cancer-related pathways linked to infection were identified. Nine genes were expressed differently between infected and uninfected women, 23 genes changed in women who cleared the infection after treatment, and 29 genes differed between women post-treatment and those never infected.
Altered genes
Among the nine most significantly altered genes between infected and uninfected women, four were linked to cancer:
- BLK proto-oncogene: A tyrosine kinase that drives cell proliferation and can contribute to tumour formation when dysregulated
- Long Intergenic Non-Protein Coding RNA 2084: A prognostic marker in head, neck, and colon cancers, influencing gene regulation tied to tumour progression
- Trichohyalin: Involved in keratin complex formation and upregulated in certain cancers
- TCL1 family AKT coactivator A: Promotes cell survival and proliferation, and is linked to T- and B-cell lymphomas
Post-treatment, certain cancer-related biological pathways became more active, particularly those involved in inflammation, tissue remodelling, and the breakdown of protective barriers in the cervix. These changes were linked to increased blood vessel formation, activation of tumour-related processes, and reduced programmed cell death (apoptosis)—a key mechanism for eliminating abnormal cells.
Triggering molecular changes
“The findings suggest that infection may trigger molecular changes that make women more vulnerable to cancer-related processes in the cervix, especially after treatment,” explains Dr. Anna Maria Mertelsmann, lead study author. “One particularly concerning observation was the downregulation of genes responsible for maintaining cervical tissue integrity, including claudins and tight junction proteins. This loss of protective function could facilitate HPV infection and persistence, a major risk factor for cervical cancer.”
“Our research shows that women who received praziquantel treatment exhibited more genetic changes linked to cancer than those with an active infection,” Dr. Mertelsmann added. “This raises critical questions about the long-term effects of treatment and highlights the need for careful post-treatment monitoring.”
Dr. Anna Maria Mertelsmann is a researcher at University Hospital Zurich and Weill Cornell Medicine, specialising in infectious diseases and molecular oncology. Her work focuses on understanding parasitic infections and their role in cancer development.
DIfficult to diagnose
This study serves as an important first step in understanding the role of S. haematobium in cervical cancer, and a larger study following 180 women over 12 months is currently underway to confirm these findings. Future research will also explore whether women who have had schistosomiasis are at greater risk of cervical cancer due to long-term HPV infections.
Dr. Mertelsmann and her team stress the need for greater awareness of Female Genital Schistosomiasis (FGS), as many women with S. haematobium are also affected by this difficult-to-diagnose condition.
“Women diagnosed with S. haematobium should be closely monitored for early signs of cervical tissue abnormalities,” she emphasised. She also suggested that additional treatments—such as anti-inflammatory or immune-modulating therapies—could help counteract the harmful effects seen after treatment. Moreover, widespread HPV vaccination could play a crucial role in reducing cervical cancer risk for women affected by schistosomiasis.
- Mertelsmann, A. M., Maganga, J. K., Lee, M. H., et al. (2025). Schistosoma haematobium infection is associated with oncogenic gene expression in cervical mucosa, with enhanced effects following treatment. Oral Presentation. ESCMID Global 2025.
- World Health Organization. (2023). Schistosomiasis. Retrieved from https://www.who.int/news-room/fact-sheets/detail/schistosomiasis
- Mertelsmann, A. M., Bowers, S. F., Wright, D., et al. (2024). Effects of Schistosoma haematobium infection and treatment on the systemic and mucosal immune phenotype, gene expression and microbiome: A systematic review. PLOS Neglected Tropical Diseases. https://doi.org/10.1371/journal.pntd.0012456






No comments yet