A low-cost technology involving nanoparticles loaded with antibiotics and other antimicrobial compounds that can be used in multiple attacks on infections by the bacterium responsible for most cases of tuberculosis has been developed by researchers at São Paulo State University (UNESP) in Brazil.

The study is reported in an article published in the journal Carbohydrate Polymers. Results of in vitro tests suggest it could be the basis for a treatment strategy to combat multidrug bacterial resistance.
According to Brazil’s Health Ministry, some 78,000 cases of tuberculosis were notified in 2022, 5% more than in the previous year and more than in any other country in the Americas. In addition to the rise in incidence, the number of cases involving multidrug-resistant strains is also growing.
The main agent of the disease is the bacillus Mycobacterium tuberculosis, one of the most lethal bacteria known to scientists. Transmission occurs via inhalation of bacilli, which migrate to the pulmonary alveoli, causing inflammation of the airways and eventually destroying lung tissue.
Use of nanotechnology
The use of nanotechnology is one of the novel treatment strategies considered most promising by scientists around the world against multidrug-resistant strains of M. tuberculosis. The UNESP study, which was funded by FAPESP, analyzed the antitubercular activity of nanoparticles comprising N-acetylcysteine (an over-the-counter supplement), chitosan (a natural compound derived from the outer skeleton of shellfish), an antimicrobial peptide originally isolated from the skin of a Brazilian frog species, and rifampicin (an antibiotic commonly used to treat tuberculosis).
The results showed that the nanoparticles significantly inhibited progression of the disease and overcame resistance to the drug without causing cell damage.
In vitro assays were performed with M. tuberculosis-infected fibroblasts, the main cells active in connective tissue, and macrophages, cells of the innate immune system and a key component of first-line defense against pathogens.
Revitalized and optimized
“Rifampicin is considered obsolete for certain strains of the bacillus, but in our study, we revitalized and optimized it with antimicrobial peptides that have been proven to help combat the disease,” said Laura Maria Duran Gleriani Primo, first author of the article and an undergraduate student at UNESP’s School of Pharmaceutical Sciences with a scientific initiation grant.
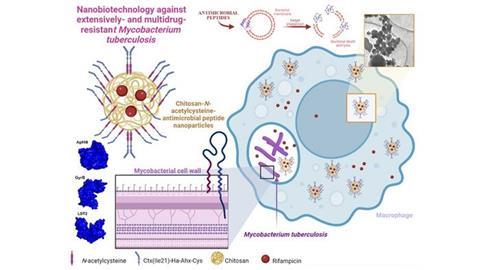
“These peptides interact with various receptors in different parts of the bacterium, in both the membrane and periplasm. We found that they revitalized rifampicin, which became even more active inside macrophages,” said Cesar Augusto Roque-Borda, joint first author of the study and a PhD candidate in UNESP’s Program of Graduate Studies in Biosciences and Pharmaceutical Biotechnology. The periplasm is a region of bacterial cells that lies between the inner cytoplasmic and outer bacterial membranes of the cell envelope.
Shorter treatment time
Conventional treatment of tuberculosis entails concomitant use of several antiobiotics for six months to about two years depending on the patient’s response and the bacterium’s resistance. The researchers expect their technique to shorten this time.
“From the study, we know it’s possible to insert a considerable concentration of antibiotic and peptides into macrophages – enough to boost the effect of the treatment,” said Fernando Rogério Pavan, last author of the article and a professor at UNESP’s School of Pharmaceutical Sciences. “Our expectations for future research include using this type of nanotechnology with other drugs and slow-release medications so that patients don’t need to take their medication every day.”
The next step will be to confirm the in vitro findings by means of in vivo trials and study the use of the nanoparticles to combat other diseases that require treatment for long periods.
Topics
- Antimicrobial Resistance
- Antimicrobials
- Bacteria
- Cesar Augusto Roque-Borda
- chitosan
- Fernando Rogério Pavan
- Infection Prevention & Control
- Innovation News
- Laura Maria Duran Gleriani Primo
- Mycobacterium tuberculosis
- N-acetylcysteine
- One Health
- Pharmaceutical Microbiology
- Rifampicin
- São Paulo State University
- The Americas
- tuberculosis







No comments yet