New research has investigated the use of metagenomic next-generation sequencing (mNGS) in diagnosing bloodstream infections (BSIs) for immunocompromised hematology patients.
Haematology patients are highly susceptible to BSIs, which can have severe consequences such as septic shock, multiple-organ failure, disseminated intravascular coagulation, and even death. An accurate and quick microbiological diagnosis of BSI is therefore essential for the control of the infection.
In the study, conducted between January 2019 and December 2020 at Tongji Hospital with the participation of BGI Genomics researcher Wenqian Zhang, peripheral blood samples were collected from 256 immunocompromised haematology patients suspected of BSI, and both mNGS and conventional microbiological tests (CMTs) were performed.
How it went
BSI diagnosis was confirmed in 189 out of 256 patients (73.8%). The detection rate of mNGS was significantly higher than that of CMTs, with mNGS identifying 187 infection cases and CMTs identifying 81. Results indicate mNGS outperformed CMT in detecting bloodstream infections.
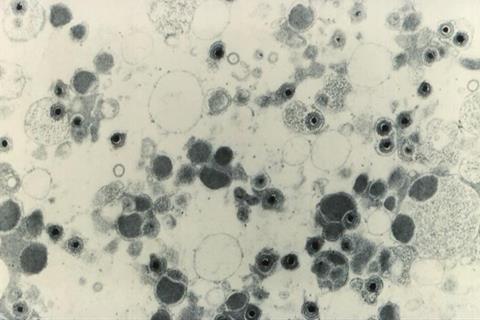
Bacteria were detected in 17 patients (6.6%), fungi in 15 patients (5.9%), rare pathogens in 4 patients (1.6%), and multiple species in 55 patients (21.5%).
Based on mNGS results, viral infection was the most frequent BSI, identified in 96 out of 256 patients (37.5%). The five most common causative viruses were CMV (31.3%), EBV (14.8%), HSV1 (11.7%), BK virus (11.7%) and HHV6B (9.4%).
The results also showed that it was more likely for patients who had undergone haematopoietic stem cell transplantation (HSCT), than those who had not, to be infected by BK virus and HHV6B.
Overall, the study, published in the Journal of Infection, highlights the potential of mNGS as a powerful tool for the rapid and accurate diagnosis of BSIs in immunocompromised hematology patients, allowing for timely and effective treatment.







No comments yet