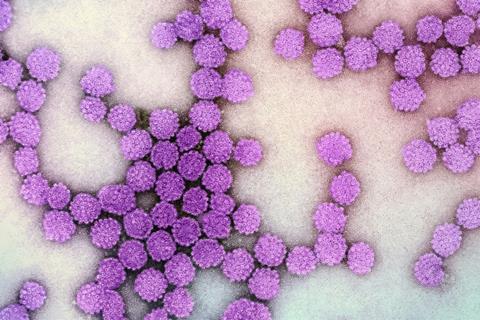
Cervical cancer, the fourth most common cancer type in women, causes approximately 350,000 deaths each year, mainly in middle- and low-income countries. Human papillomavirus (HPV) infection is known to cause 95% of these cases.
Public health authorities in 37 countries currently vaccinate girls between nine and 14 years of age, before they typically start sexual activity.
HPV is also known to increase the risk of genital warts and cancers of the penis, anus, mouth, and throat in infected men, which is one of the reasons why the WHO and the US Center for Disease Control (CDC) advise that boys, too, should be routinely vaccinated against it. However, the full suite of potential effects of HPV in men and boys is still unknown.
READ MORE: Researchers develop noninvasive urine test for early detection of cervical cancer virus proteins
READ MORE: Researchers identify new genetic risk factors for persistent HPV infections
“Here we show that genital HPV infection is very prevalent in men, with variable effects on semen inflammation and sperm quality according to the infecting viral genotype,” said Dr Virginia Rivero, a professor at the Universidad Nacional de Córdoba in Argentina, and the senior author of a new study in Frontiers in Cellular and Infection Microbiology.
“Specifically, infections caused by high-risk HPV genotypes appear to have more negative effects on male fertility and the immune system’s ability to clear the infection.”
Implicated in cancers
More than 200 different HPV genotypes have been identified, typically classified in high-risk (HR-HPV) and low-risk (LR-HPV) genotypes. HR-HPV can be detected in approximately 100% of cervical cancers in women and a high percentage of anal, genital, and mouth and throat cancers in women and men. LR-HPV is typically detectable in abnormal but benign cervical cells in women and warts on the surface of the larynx and genitals in both sexes, but without causing cancer.
Rivero and colleagues studied the effects of HPV in a cross section of the male population in Argentina: 205 adult male volunteers who attended a single urology and andrology clinic for initial fertility assessment or problems of the urinary tract between 2018 and 2021. None had been vaccinated against HPV.
Study of samples
The volunteers donated a sample of their ejaculate, and the presence or absence of HPV and other sexually transmitted infections were determined by PCR. Among the 205 individuals analyzed, 19% tested positive for HPV. Specifically, 20 men were classified as positive for HR-HPV, while 7 were identified as positive for LR-HPV.These HPV-positive individuals were compared to 43 men with no infections detected. A further 12 men were found to be HPV positive, but their genotype couldn’t be determined due to low viral loads.
Most HPV positive men were infected with only a single genotype, but three men carried two genotypes simultaneously.
Routine analysis
First, the researchers studied the semen samples with a battery of routine analysis methods, as recommended by the WHO. Following these criteria, they found no evidence of a difference in semen quality between the three groups.
However, this apparent suggestion of normal fertility in HPV-infected men proved to be far from the full picture. When Rivero and colleagues examined the samples with more focused, high-resolution methods, they were surprised to find that HR-HPV positive men had significantly lower counts of CD45+ white blood cells (leukocytes) in their semen. They also found evidence that sperm of HR-HPV positive men may suffer frequent damage from oxidative stress, judging by their elevated production of reactive oxygen species (ROS).
While low levels of ROS are a product of normal sperm function, elevated levels can lead to rupture of the cell membrane, breaks in DNA, and uncontrolled and unprogrammed cell death. Indeed, the researchers showed that HR-HPV positive men had a higher percentage of dead sperm.
Increased sperm death
“We concluded that men infected with HR-HPV, but not men infected with LR-HPV, show increased sperm death due to oxidative stress and a weakened local immune response in the urogenital tract,” said Rivero.
“These results suggests that HR-HPV positive men could have impaired fertility.”
Rivero et al. explained the observed lower count of immune cells in the semen of HR-HPV positive men from the known ability of HPV to evade an immune response. This would lead to a reduced movement of leukocytes to the site of HPV infection and their impaired ability to clear this infection.
“Our study raises important questions about how HR-HPV affects sperm DNA quality and what implications it has for reproduction and offspring health. It’s important to understand the biological mechanisms underlying these effects. And, given that sexually transmitted co-infections are quite common, we plan to explore whether bearing HPV infection alongside other STIs influence these outcomes,” said Rivero.







No comments yet