Scientists in the La Jolla Institute for Immunology (LJI) Center for Vaccine Innovation are working to develop new measles vaccines and therapeutics that stop this fusion process. The researchers recently harnessed an imaging technique called cryo-electron microscopy to show—in unprecedented detail—how a powerful antibody can neutralize the virus before it completes the fusion process.
Fusion in action
“What’s exciting about this study is that we’ve captured snapshots of the fusion process in action,” explains LJI Professor, President and CEO Erica Ollmann Saphire, Ph.D., who co-led the Science study with Matteo Porotto, Ph.D., Professor of Viral Molecular Pathogenesis (in Pediatrics) at Columbia University.
“The series of images is like a flip book where we see snapshots along the way of the fusion protein unfolding, but then we see the antibody locking it together before it can complete the last stage in the fusion process. We think other antibodies against other viruses will do the same thing but have not been imaged like this before.”
Indeed this work may prove important beyond measles. Measles virus is just one member of the larger paramyxovirus family, which also includes the deadly Nipah virus. Nipah virus is known for being less contagious but causing a much higher mortality rate than measles.
“What we learn about the fusion process can be medically relevant for Nipah, parainfluenza viruses, and Hendra virus,” says study first author and LJI Postdoctoral Researcher Dawid Zyla, Ph.D. “These are all viruses with pandemic potential.”
Urgent need
Measles is a highly contagious, airborne disease that tends to strike children the hardest. Despite extensive vaccine efforts, the virus remains a major health threat. According to the World Health Organization and the U.S. Centers for Disease Control, measles caused around 136,000 deaths globally in 2022, with recent outbreaks in over a dozen U.S. states. The victims were mostly children under age five who were unvaccinated or undervaccinated.
“Measles causes more childhood deaths than any other vaccine-preventable disease, and it’s also one of the most infectious viruses known,” says Saphire.
It’s not just young children at risk, explains Zyla. “The current vaccine works well, but it cannot be taken by pregnant people or people with compromised immune systems,” Zyla says.
Search for antibodies
There is no specific treatment for measles, so researchers are looking for antibodies to use as an emergency treatment to prevent severe disease.
To better understand how the measles virus fuses with cells, the LJI team turned to an antibody called mAb 77. Researchers have found that mAb 77 targets the measles fusion glycoprotein, the piece of viral machinery measles uses to enter human cells via a specialized process called fusion.
Could mAb 77 work as a therapeutic antibody against measles? To find out, the LJI scientists investigated exactly how the antibody combats the virus.
Membrane fusion interrupted
The LJI team needed to engineer a version of the measles fusion glycoprotein—a harmless fragment of the virus—stable enough to image with a cryo-electron microscope. To do this, Zyla worked closely with scientists in Porotto’s laboratory at Columbia University.
Porotto’s group had uncovered some strange mutations in a measles variant that attacked peoples’ central nervous systems. This mutated variant had some weak points in its fusion glycoprotein structure. To compensate, the virus had evolved special stabilizing mutations. “The virus has to mutate to go into the brain, but then it needs these stabilizing mutations to compensate,” says Porotto.
Thanks to these discoveries at Columbia, Zyla had a handy blueprint for engineering a fusion glycoprotein with these same stabilizing mutations. This new fusion glycoprotein could be mass produced in cell culture, and it was sturdy enough for structural investigations.
Good yields
“We got extremely good yields for the glycoprotein, which also enabled us to do structural biology and biochemical and biophysical studies,” says Zyla.
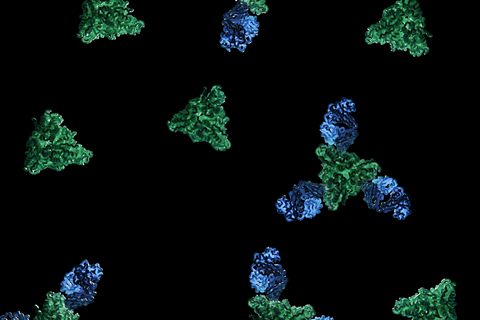
Next, the researchers started capturing images with the help of the LJI Cryoelectron Microscopy Core. The new images showed the fusion glycoprotein together “in complex” with mAb 77.
The researchers found mAb 77 arrests the virus in the middle of the fusion process—when fusion glycoprotein is already part way done “folding” into the right conformation to complete membrane fusion. At last, the researchers could see exactly how mAb 77 locks together pieces of the fusion glycoprotein to prevent viral infection.
“It was striking to see what this intermediate step in the fusion process actually looks like,” says Zyla.
Next steps
Now that they know how mAb 77 works, the researchers hope the antibody could be used as part of a treatment cocktail to protect people against measles or to treat people with active measles infection.
In a follow-up experiment, the researchers showed that mAb 77 provided significant protection against measles in cotton rat models of measles virus infection. Cotton rats pretreated with mAb 77 prior to measles virus exposure showed either no infection or reduced signs of infection in their lung tissue.
Going forward, Saphire and Zyla are interested in studying different antibodies against measles. “We’d like to stop fusion at different points in the process and investigate other therapeutic opportunities,” Zyla says.
Zyla also plans to continue working closely with measles researchers at Columbia University. “The combination of structural biology expertise from LJI and cell biology and virology expertise from Columbia was key to pushing this project forward,” says Zyla.







No comments yet