Researchers at the Experimental and Clinical Research Center of Max Delbrück Center and Charité – Universitätsmedizin Berlin (ECRC) have found that different anatomical sections of the gastrointestinal tracts of mice carry different compositions of microbial communities. Moreover, the specific makeup of the microbiota can influence the type and abundance of immune cells in any particular region.
The study, which was published in Gut Microbes, maps the complex spatial organization of immune cells and microbial communities, providing a tool for studying the interaction between gut microbes and inflammatory diseases.
READ MORE: Researchers develop tool that measures health of a person’s gut microbiome
READ MORE: Switching to vegan or ketogenic diet rapidly impacts immune system - and gut microbiome
Previous research has hinted at the existence of “hotspots” along the GI tract where specific immune cells and microbes might interact more intensely. But no one had systematically investigated this across the entire gut, says Dr. Hendrik Bartolomaeus, in the Immune-Microbial Dynamics in Cardiorenal Disease lab of Dr. Nicola Wilck, and an author of the study. “We were motivated by a simple question: How are immune cells organized along the gut, and how does the microbiome influence this organization?”
Microbial communities shape the immune system
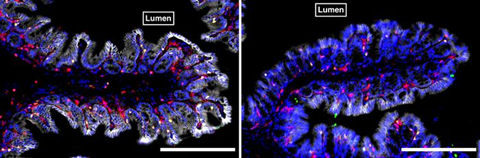
The researchers compared the GI tracts of germ-free mice with conventionally colonized mice by dissecting their intestines into segments, and then extracting microbial DNA. They used metagenomic sequencing to identify all the bacterial species present. Concurrently, they isolated immune cells from the segments and analyzed them using flow cytometry, a commonly used technique to identify and quantify different immune cell types based on specific cellular markers.
They found that not only did the microbial communities in the GI tract of conventional mice vary depending on location. But this also significantly influenced the distribution and type of immune cells found along the gut. For instance, adaptive immune cells, which are acquired after exposure to antigens – foreign substances that induce an immune response – were more prominent in the lower parts of the intestine, while innate immune cells were more abundant in the upper segments. This pattern was severely disturbed in germ-free mice, which lack bacterial antigens in their intestine.
Go-to app
Harithaa Anandakumar, PhD student and lead author of the study, then categorized the immune cells according to whether their presence and abundance is influenced only by location, by an interaction with the microbiota at that location, or both. She then created an app that summarizes the information. “We built a go-to app so that anyone who is interested in a specific immune cell type can look it up and see where it’s most abundant in the gut and whether it is influenced by the microbiome, the location, or an interaction of both.”
Such a resource had been lacking, says Wilck, who is also a specialist at Charité’s Department of Nephrology and Medical Intensive Care. Now any scientist working with mouse models can use it. His own lab studies how immune cells travel from the gut into tissues and organs in various mouse models of disease. “We can now use this resource to study whether the immune cells we find in organs damaged by hypertension or kidney disease come from the gut,” he says.







No comments yet