The flu virus is constantly evolving, meaning immunity from past infections or vaccinations may not fully protect against new strains. These mutations are why last year’s flu vaccine may no longer be effective, requiring annual updates to keep up with the latest variants.
But what if our immune system could recognise a broader range of flu viruses, providing longer-lasting protection? New research suggests that certain immune cells, a subset of T cells, might hold the key.
Research led by the Peter Doherty Institute for Infection and Immunity (Doherty Institute) and Monash University has uncovered how specific T cells, which play a critical role in fighting infections, can detect multiple flu strains, even those that have evolved over a century. This process, known as cross-reactivity, could be crucial in developing more effective immunity against influenza.
READ MORE: Mutation could facilitate H5N1 bird flu virus infection and potential transmission in humans
READ MORE: H5 influenza vaccines: what needs to be done to reduce the risk of a pandemic
In the study, published in Science Immunology, researchers analysed samples from individuals with different flu viruses and identified a subset of T cells that recognise a particular protein present in influenza A viruses, from the 1918 Spanish flu to the latest 2024 H5N1 strains.
Multiple variants
The University of Melbourne’s Dr Oanh Nguyen, Senior Research Fellow at the Doherty Institute and co-author of the study, explained the molecular mechanisms that enable these T cells to recognise multiple influenza variants.
“We tested how people’s T cells respond to a specific part of the influenza virus that changes frequently. Over the last 100 years, this region has evolved into 12 different forms,” said Dr Nguyen.
“We found that some individuals have T cells that can recognise up to nine of these variants, while others have T cells that can only detect a couple.”
Molecular details
Professor Jamie Rossjohn, Immunologist at Monash University and co-senior author of the study, explained how the team uncovered the molecular details behind this immune response.
“This work reveals an untapped ability of the immune system to respond to flu viruses, even as they change over time,” said Professor Rossjohn.
“We used an advanced technique called crystallography to determine how T cells see flu viruses at the molecular level. We observed specific interactions between the T cells and the flu proteins that determine why some T cells are better at detecting a wide range of strains than others.
“While our findings deepen our understanding of how T cells react to changing flu viruses, they are also highly relevant for understanding immune responses to other rapidly evolving viruses such as SARS-CoV-2.”
Universal vaccine
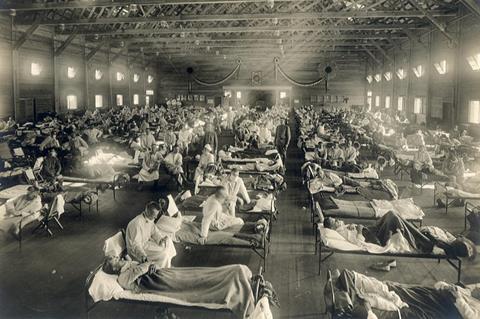
The flu remains a major global health threat. According to the WHO, flu causes 3 to 5 million cases of severe illness and up to 650,000 respiratory deaths each year, particularly among vulnerable populations.
The University of Melbourne’s Professor Katherine Kedzierska, Head of the Human T cell Laboratory at the Doherty Institute, said a universal vaccine, one that protects against multiple strains for longer periods, would be a game changer.
“This research is hugely significant. It shows how certain T cells can recognise multiple flu strains, which is a big step towards understanding universal protective immunity – not just for the flu, but potentially for other viral diseases too,” said Professor Kedzierska.
“Harnessing these cross-reactive responses could be the key to a vaccine that offers longer-lasting protection and reduces the risk of future flu pandemics.”







No comments yet