A new study has highlighted the discharge of untreated hospital effluent to the environment as a major driver of multidrug resistance among the microbial community.
The research, presented at the recent Letters in Applied Microbiology ECS Research Symposium, found that hospital wastewaters are primary hotspots for the selection of resistant microbes, with several types of antimicrobials being flushed frequently and inducing high selection pressure in the bacterial community.
Researcher Sunday Augustine, of Federal University of Technology in Minna, presented the research, ‘Assessment of multidrug-resistant gram-negatives bacteria associated with hospital wastewater in Minna, Nigeria’.
Hospital wastewater
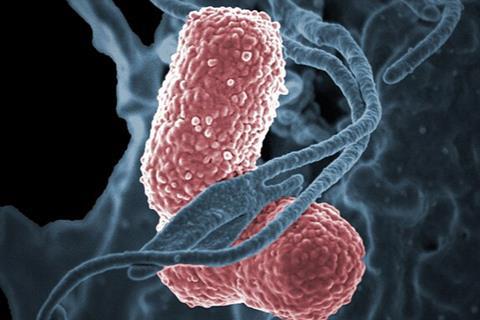
“My research was focused on the assessment of hospital wastewater to determine the multidrug resistance patterns of the bacteria isolated from designated hospitals in Minna. The study identified a total of 24 bacteria of four different genera, including Proteus mirabilis, Salmonella enterica, Pseudomonas aeruginosa, and Klebsiella pneumoniae,” he said.
“The study concluded that hospital sewage serves as a hotspot for antibiotic-resistant bacteria, contributing to their spread in the environment. It also emphasized the significance of hospital wastewater as a source of MDR organisms, highlighting the need for appropriate treatment of hospital wastewater and other clinical settings to prevent the spread of MDR bacteria.”
The current research revealed that the discharge of untreated hospital effluent to the environment was the major driver of multidrug resistance among microbial community, Mr Augustine said.
Sub-lethal dose
“The exposure of bacteria to sub-lethal dose of antimicrobials and chemical substances allow the bacteria to undergo mutation giving rising to new strains of bacteria which are resistant to the antimicrobial agents. These new strains can disseminate the resistance genes in the environment to other bacteria through horizontal gene transfer.
“The study further necessitated the treatment of hospital wastewater with bio- flocculants prior to their discharge to the environment. Treating the hospital wastewater with bio-flocculants help convert the substance into harmless form before discharge to the environment. This helps to prevent development and acquisition of antibiotic resistant genes through natural selection pressure in the environment.”
Samples from hospitals
The research involved collecting six wastewater samples from the General hospital, Standard hospitals, and the Federal University of Technology Minna Clinics in Minna, Niger State. Samples were collected in sterile conical flask and were transported aseptically to the Microbiology laboratory at Federal University of Technology, Minna for further analysis.
The collected wastewater samples were processed to concentrate the bacteria. This involved centrifugation at a low speed to separate the bacterial cells from the liquid portion. The resulting pellet was re-suspended in a smaller volume of sterile saline solution.
The resuspended bacterial cells were streaked first on Nutrient agar, then onto selective agar plates, including MacConkey agar, Salmonella-Shigella Agar (SSA) which promote the growth of various Gram-negative bacteria.
Colony growth
These plates were then incubated at an appropriate temperature (37°C) for 24 hours to allow the growth of colonies. After incubation, the MacConkey agar, SSA, and EMB agar plates were observed for the presence of bacterial colonies. The colonies were examined for their size, shape, color, texture, and other physical characteristics.
A bacterial sample was picked from the plates using a sterile wire loop and spread onto a microscope slide. The slide is heat-fixed to attach the bacteria to the slide. The slide is flooded with crystal violet stain, which stains all the bacteria purple.
The slide was rinsed with water after 30 seconds and then flooded with iodine, which acts as a mordant for 1 minute to fix the stain in the bacterial cell walls. The slide was rinsed again with water and then flooded with 75% alcohol for 5 seconds, which acts as a decolorizing agent. This step removes the stain from some bacteria, but not others. The slide was rinsed again with water and then flooded with safranin, which stains the decolorized bacteria pink. The slide was rinsed with water, air-dried, and then examined under x100 objective lens of the microscope.
After incubation, individual colonies were picked from the agar plates and subjected to various biochemical tests, including oxidase test, catalase test, indole test, methyl red and a host of others to identify the gram-negative bacteria.
Indole Methyl Red Citrate Utilization Test (IMVIC)
A tube of tryptone broth was inoculated with a pure culture of the test organism and incubated at 37°C for 24 hours. After incubation, a few drops of Kovac’s reagent were added to the tube. A red color was observed, indicating a positive indole test.
A tube of MR-VP broth was inoculated with a pure culture of the test organism and incubated at 37°C for 24 hours. After incubation, a few drops of the MR reagent were added to the tube. A red color was observed, indicating a positive MR test.
A second tube of MR-VP broth was inoculated with a pure culture of the test organism and incubated at 37°C for 24 hours. After incubation, a few drops of the VP reagents were added to the tube. A red color was observed, indicating a positive VP test.
A tube of Simmons citrate agar was inoculated with a pure culture of the test organism and incubated at 37°C for 24 hours. After incubation, the color of the agar was observed. A change from green to blue was noted, indicating a positive citrate utilization test.
More tests
A loopful of the test organism was placed on a glass slide. A few drops of 3% hydrogen peroxide were added to the bacterial culture. The presence of bubbles indicated a positive catalase test.
A loopful of the test organism was placed on an oxidase test strip. The development of a blue-purple color within 10-30 seconds indicated a positive oxidase test.A TSI (Triple Sugar Iron) agar slant was inoculated with the test organism using a straight wire inoculation technique. The slant was then stabbed with the inoculating loop to reach the bottom of the tube.
After incubation, the results were interpreted based on the color changes in the medium, gas production, and H2S production.
Motility test
A semisolid agar tube was inoculated with the test organism using a straight wire inoculation technique. After incubation, the growth pattern of the bacteria was observed. A diffuse growth pattern indicated motility, while a localized growth pattern indicated non-motility.
The identified Gram-negative bacteria were tested against ten antibiotics for their susceptibility to various antibiotics using the Kirby-Bauer disk diffusion method. This allowed the determination of the bacteria’s resistance patterns and the selection of appropriate antibiotics for further characterization.
A pure culture of the test organism is obtained and grown in a nutrient broth or agar. A standardized inoculum of the bacterial culture is prepared and spread onto a Mueller-Hinton agar plate. Antibiotic discs containing different antibiotics are placed onto the agar plate, and the plate is incubated at 37°C for 24 hours. After incubation, the diameter of the zone of inhibition around each antibiotic disc is measured and compared to a standardized chart to determine the susceptibility of the bacteria to each antibiotic. The results are interpreted as susceptible, intermediate, or resistant, based on the size of the zone of inhibition.
Fascinating discovery
All the isolates were found to be multi-drug resistant, with the Multiple Antibiotic Resistance (MAR) index ranging from 0.2 to 1.0%. Klebsiella pneumoniae and Pseudomonas aeruginosa showed the highest resistance, at 100%, to the ten antibiotics tested, while the other isolates exhibited resistance to at least three or more antibiotics. The highest resistance was observed against Amoxicillin (100%), followed by Augmentin (98%), Septrin (95%), and Pefloxacin (25%). The study concluded that hospital sewage serves as a hotspot for antibiotic-resistant bacteria, contributing to their spread in the environment.
Multidrug resistance
“Multidrug resistance is a great threat to public health. The discharge of untreated hospital effluent to the environment further exacerbates the emergence of bacterial strains that are resistant to three or more classes of antibiotics,” Mr Augustine said.
“This necessitated the development of innovative treatment measures for the wastewater to prevent the selection of bacterial strains in the environment.”
Future research using Molecular Antibiotic Resistance Gene Analysis will build on the investigation of the presence and diversity of antibiotic resistance genes in the isolated bacteria. Researchers will also develop, design and test innovative technologies to efficiently remove MDR bacteria and antibiotic genes from hospital wastewater, and increase the number of hospital wastewater samples to better represent the region.
The Letters in Applied Microbiology Early Career Scientist Research Symposium was held at University of the West of England (UWE) in Bristol, UK, on 15 May 2024. To find out more about forthcoming AMI events, visit the event page.
Topics
- Antimicrobial Resistance
- Applied Microbiology International
- Bacteria
- Community
- Federal University of Technology Minna
- Infectious Disease
- Klebsiella pneumoniae
- Microbiological Methods
- Middle East & Africa
- One Health
- Proteus mirabilis
- Pseudomonas aeruginosa
- Research News
- Salmonella enterica
- Sunday Augustine
- Wastewater & Sanitation







No comments yet