A scientific team from the Yong Loo Lin School of Medicine at the National University of Singapore (NUS Medicine) and Monash University, Australia, has engineered a COVID-19 vaccine that induced – in pre-clinical models – very long-lasting, protective immunity against SARS-CoV-2 virus with a single-shot immunisation.
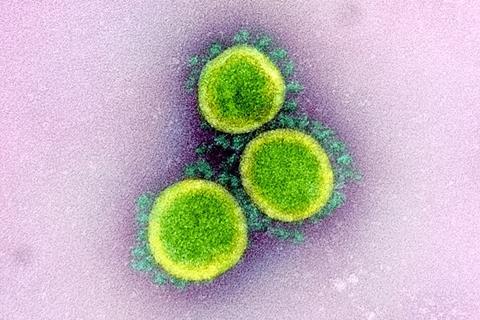
In an on-going, four-year collaboration, the team leveraged on a novel vaccine platform to fuse the receptor-binding domain (RBD) from the spike protein of the SARS-CoV-2 virus to the Clec9A antibody. The Clec9A antibody targets a specific subset of dendritic cells, a specialised type of immune cells found in tissues such as the skin, which are responsible for initiating immune responses in our body.
Upon a single shot immunisation of the Clec9A-RBD antibody construct, the team monitored the immune responses in pre-clinical models over 21 months, and found no signs of declined immunity. In contrast, it observed that the quality of the immune response (the neutralising antibody response, in particular), was associated with increased protection over time.
The study was published in Molecular Therapy , which is part of Cell Press.
Waning immunity
This new Clec9A targeting technology may potentially address the issue of waning COVID-19 vaccine immunity, and eliminate the need for repeated booster jabs, particularly for people aged 60 and over, medically vulnerable individuals and their caregivers.
“The results that we see in this study are very promising, and we are confident that the work performed in pre-clinical models is highly translatable to humans,” said Associate Professor Sylvie Alonso, Principal Investigator of this study. “Indeed, a human equivalent of this immune cell subset exists, and our collaborator, Associate Professor Mireille Lahoud, at Monash University is developing this approach towards future human application.
Associate Professor Lahoud said: “This study demonstrates the strength of our platform targeting specialised immune cells for vaccine improvement, and exemplifies the power of international research collaborations spanning basic discoveries to translational studies.”
Exceptional durability
Current Messenger RNA (mRNA) COVID-19 vaccines have been reported to demonstrate peak effectiveness of 162% after three weeks, post-jab, before declining to nine per cent after nine months. Protection from booster doses has been reported to wane, dropping from 260 per cent one month after the booster dose to 13 per cent at nine months.
“Our teams in NUS Medicine and Monash University foresee that the exceptional durability of the immune responses induced by the Clec9A targeting technology, when used as a booster vaccine strategy, may address the shortcoming of current mRNA vaccines, chief of which is the rapid waning of immune responses,” Associate Professor Alonso, who is also co-Director of the Infectious Diseases Translational Research Programme at NUS Medicine said.
“We are now evaluating our vaccine candidate as a booster vaccine in mRNA-vaccinated pre-clinical models. We hope to demonstrate that this booster approach will induce long-term protective immunity, and avoid the need of multiple (annual) booster shots.
“Beyond COVID19, this versatile, rapidly-deployable vaccine platform shows promising potential to be part of the pandemic response against Disease X caused by an unknown pathogen in the future.”
Universal flu vaccine candidate
This latest breakthrough follows closely on the heels of the team’s 2022 research, published in the Proceedings of the National Academy of Sciences of the United States of America (PNAS). Back then, it leveraged on the Clec9A targeting vaccine platform to deliver the universal influenza vaccine candidate M2e.
M2e is notoriously known to be unable to induce strong and durable immune responses. The team demonstrated that a single-shot immunisation of the Clec9A-M2e construct triggered long-lasting immune responses to effectively protect against multiple strains of the flu. It effectively removes a major bottleneck in the clinical development of M2e-based vaccine candidates.







No comments yet