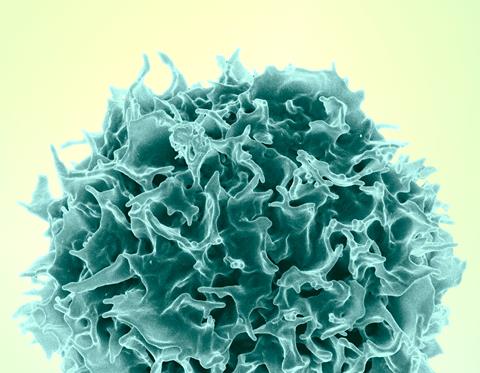
A clinical trial sponsored by the National Institutes of Health (NIH) has launched to examine the safety and acceptability of a novel rectal HIV microbicide douche containing the antiretroviral drug tenofovir. This “on-demand” HIV prevention approach involves using the microbicide prior to a potential exposure from receptive anal intercourse.
Several forms of HIV pre-exposure prophylaxis (PrEP) are in use in the United States and globally, namely daily oral pills, long-acting injections, and a monthly vaginal ring.
READ MORE: Isolated viral load test may generate false positive results for people using long-acting PrEP
READ MORE: Long-acting injectable cabotegravir for HIV prevention is safe in pregnancy
The Centers for Disease Control and Prevention advises that gay, bisexual and other men who have sex with men who meet certain criteria can take “on-demand” oral PrEP around the time of sex to prevent HIV acquisition, but there is insufficient evidence to support its use in other populations.
Rectal microbicides are another HIV prevention method being explored for use in an “on-demand” manner to expand the choices available to eligible people who engage in receptive anal intercourse and who stand to benefit from using PrEP.
On-demand douche
The clinical trial will enroll about 150 male adults who have regular experience using an unmedicated rectal douche before receptive anal intercourse. Participants will each receive “on-demand” tenofovir rectal microbicide douche during one two-month period and on-demand oral PrEP with tenofovir disoproxil fumarate and emtricitabine in another two-month period. All particpants will be monitored closely for safety. The study also will assess participants’ experience using their assigned PrEP method, including measures of acceptability, adherence, and method preference. The study will take place at eight sites in the United States.
While HIV incidence is slowly decreasing in the United States, 67% of U.S. HIV diagnoses from 2018-2022 were among gay, bisexual, and other men who have sex with men, pointing to the need for expanded HIV prevention options. The mid-stage study is sponsored NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and implemented through the NIH-funded HIV Prevention Trials Network (HPTN). NIH remains committed to developing safe and effective HIV prevention methods that people need, want, and are able to use.
More information about this study, also known as HPTN 106, is available at ClinicalTrials.gov under identifier NCT06560684.






No comments yet