A new study published in The Lancet HIV reveals gaps in knowledge surrounding the prevention of HPV-related cancers in people living with HIV and outlines future research priorities. A literature review, conducted by a team of international experts underscores the need for further research and highlights existing disparities in healthcare for this vulnerable population.
HPV-related cancers are preventable, primarily through vaccination. However, a Professor of Epidemiology at the University of Tartu and one of the study’s authors, Anneli Uusküla, said that the study found a lack of evidence on the effectiveness of the HPV vaccine in HIV-positive individuals who were vaccinated in childhood before becoming sexually active.
READ MORE: Panel issues first guidelines to prevent anal cancer in people with HIV
READ MORE: HPV vaccine prevents most cervical cancer cases in more deprived groups, major study shows
“We assume that there is at least a partial effect among HIV-positive individuals similar to that observed in HIV-negative individuals. Though, the weaker immune response to vaccination in people living with HIV compared to the general population warrants further investigation and clinical consideration,” said Uusküla.
Critical role of screening
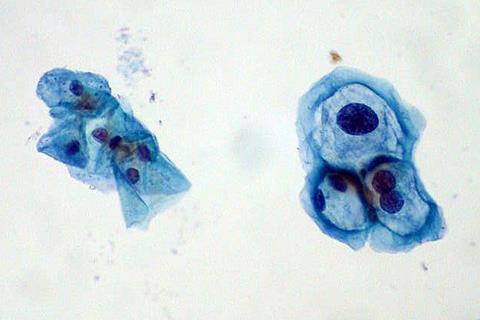
While the HPV vaccine is most effective when administered around 11-12 years old, a substantial proportion of people living with HIV acquire the virus later in life, emphasizing the critical role of screening. Cervical cancer is currently the only HPV-related cancer with an effective screening program.
While highly effective in the general population, its efficacy in preventing cervical cancer among HIV-positive individuals has not been directly proven. To date, there are no established screening programs for other HPV-related cancers, including vulvar, penile, vaginal, and oral cancers, and no evidence supports their effectiveness in cancer prevention.
“One randomized controlled trial has proven the effectiveness of anal cancer screening for cancer prevention in people with HIV,” added Uusküla.
Prevention strategies
The study also explored potential future prevention strategies. A large number of HPV infections do not lead to cancer and resolve spontaneously. Researchers are working to identify markers that can predict which HPV infections and precancerous lesions are more likely to progress to cancer, allowing for more targeted interventions. How can we identify those who are most at risk of cancer? “Currently, various molecular triage methods are being tested, and a lot of information is coming from those studies.”
People who have had one HPV-related cancer are at higher risk of developing another. Therefore, it makes a lot of sense to screen them for all HPV-related cancers at once. The development of liquid biopsies holds promise for earlier and more accurate detection of HPV-related cancers. Additionally, direct-acting anti-HPV treatments are being developed, offering hope for treating HPV infections before they progress to cancer.
Antiretroviral therapy
Antiretroviral therapy plays a crucial role for people living with HIV. “When they adhere to antiretroviral therapy, it helps maintain immune system function and may partially mitigate the risk of HPV-related cancers in this population,” explained Uusküla. Evidence suggests that antiretroviral therapy can reduce the risk of cervical, penile, and anal cancers, but further research is needed to determine its effectiveness in preventing vulvar and vaginal cancers.
The study “Prevention and control of HPV-related cancers in people living with HIV” highlights the urgent need for increased research to understand the complexities of HPV-related cancer prevention in people living with HIV.
“Healthcare providers need to be aware of the unique challenges faced by this population and advocate for improved access to vaccination, screening, and treatment. Policymakers must allocate resources to develop targeted public health programs and innovative strategies to improve the prevention of HPV-related cancers in people living with HIV. Ultimately, empowering individuals with HIV to make informed decisions about their health and advocate for enhanced access to preventative and care services is crucial,” said Uusküla.







No comments yet