A new study from the University of Pittsburgh Center for Vaccine Research published today in the Journal of Experimental Medicine describes a previously unappreciated role for a class of immune cells in the early stages of tuberculosis (TB) infection.
The researchers found that innate CD8+ lymphocytes – a subtype of white blood cells involved in rapid immune response – are essential for curbing the disease. They also discovered that an inflammatory molecule called Interleukin-15, or IL-15, plays an important role in infection control and could potentially be used to boost the efficacy of existing and future TB vaccines.
“This is an unusual finding,” said senior author JoAnne Flynn, Ph.D., distinguished professor and chair of microbiology and molecular genetics at Pitt. “No one before us has shown that CD8+ lymphocytes make a difference early in the infection in a translatable non-human primate model, but our findings suggest that these innate immune cell populations are actually playing an important role in restraining the initial infection.”
Lung disease
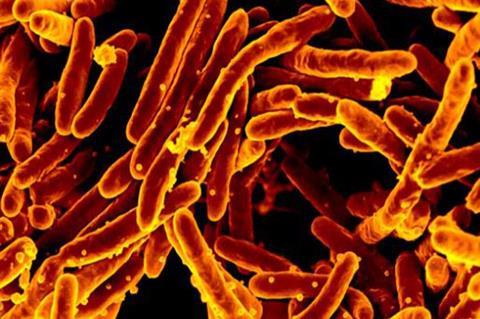
Tuberculosis, or TB, is an airborne lung disease caused by a bacterium called Mycobacterium tuberculosis. After entering the lung, these bacteria bury deep into the tissue and begin to spread, causing the body to launch an immune response and build up clumps of immune cells surrounding the bacteria, called granulomas, in an effort to control the infection and minimize damage to the lungs.
The immune response over the course of tuberculosis infection has two phases. The first six weeks after the infection are characterized by the influx of quick-acting immune cells that rush to the site of infection, be that the airways or the lung, to kill the bug and limit the damage quickly, by all means necessary.
Unlike the early innate immune response, the adaptive immune response that emerges after eight to 10 weeks of infection is more fine-tuned and aimed at precisely targeting the specific infection-causing pathogen and killing it as efficiently as possible. In general, though, the exact dynamics of the immune response in tuberculosis, and the role of fast-acting CD8+ lymphocytes was unclear.
Faster spread
Flynn and her team found that the infection was developing a lot faster and spreading further in macaque monkeys whose innate CD8+ cells were depleted than in monkeys whose total CD8+ T cell population was intact, or whose adaptive CD8+ T cells were removed, suggesting that innate CD8+ cells play a crucial role in limiting the infection in its early stages.
Using a technique called bacterium barcoding, researchers tracked the lineages of bacterial granulomas that formed over the course of the disease. In animals lacking innate CD8+ cells, researchers identified more bacterial dissemination across lungs and lymph nodes, suggesting that innate CD8+ cells create a “bottleneck,” preventing bacteria from establishing active infection.
Curiously, researchers found that in monkeys with depleted innate CD8+ cells, other immune cells tried to take over the function of fast responders, probably in response to IL-15. But because those cells lack the natural machinery that would enable them to deliver molecules that could kill the bacterium, the infection-clearing immune response was incomplete.
Next steps
As a next step in their research, scientists are studying whether IL-15 administered together with an existing TB vaccine can increase protection and make the vaccine more effective.
This study was a collaboration between Flynn’s lab and Philana Ling Lin, M.D., of UPMC Children’s Hospital of Pittsburgh, Dr. Alex Shalek, Ph.D., of the Massachusetts Institute of Technology, and Sarah Fortune, M.D., of Harvard University.
This research was funded by National Institutes of Health grants R56 AI139053, K12 HL143886 and 75N93019C00071, the Bill and Melinda Gates Foundation, Harvard University Center for AIDS Research (P30 AI060354) and the Harvard Clinical and Translational Science Center (KL2 TR002542).







No comments yet