An advanced type of MRI uncovers significant lung abnormalities in children and adolescents with long COVID, according to a new study published today in Radiology, a journal of the Radiological Society of North America (RSNA).
Post-COVID-19 condition, commonly known as long COVID, can affect individuals of all ages and is diagnosed when symptoms persist for more than 12 weeks after an initial COVID-19 infection. Children and adolescents typically experience a milder form of the condition, but common symptoms such as chronic fatigue, headaches and poor concentration can negatively impact school performance and social activities.
READ MORE: Scientists discover molecular ‘fingerprint’ of Long Covid in children’s blood
READ MORE: Study: Long COVID symptoms in children vary by age
While chest CT is frequently used to diagnose and monitor lung function of adults with long COVID, it is not typically recommended in children because it exposes the patient to ionizing radiation and may require injection of a contrast agent.
Young patients with suspected long COVID are typically evaluated with pulmonary function tests, echocardiography and reviews of medical history. Unfortunately, conventional pulmonary tests often show normal lung and cardiac function, even in symptomatic patients.
Persistent symptoms
“Parents should understand that their children’s persistent symptoms after COVID-19 may have a measurable physiological basis, even when standard medical tests appear normal,” said lead study author Gesa H. Pöhler, M.D., a senior physician in the Department of Diagnostic and Interventional Radiology at Hannover Medical School in Germany.
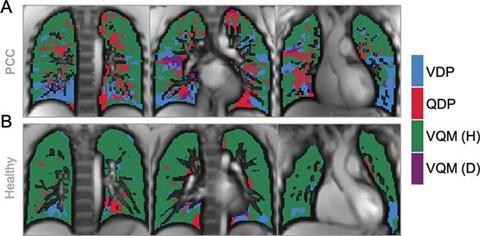
The researchers employed phase-resolved functional lung (PREFUL) MRI. This advanced MRI technology can analyze lung ventilation (air movement in and out of the lungs) and perfusion (blood flow through the lungs). PREFUL MRI doesn’t require the use of radiation or intravenous contrast agents and can be done while the patient breathes freely, making it a suitable procedure for children.
“Our research provides the first comprehensive evidence of measurable regional lung perfusion abnormalities in pediatric post-COVID-19 condition using radiation-free, contrast-free lung imaging,” Dr. Pöhler said.
Reduced blood flow
For the prospective study, conducted between April 2022 and 2023, the researchers enrolled 54 patients ranging in age from 11 to 17 years. Half of the patients were diagnosed with long COVID, and the other half were healthy controls. A self-reported assessment called the bell score was used to assess symptom severity in patients with long COVID.
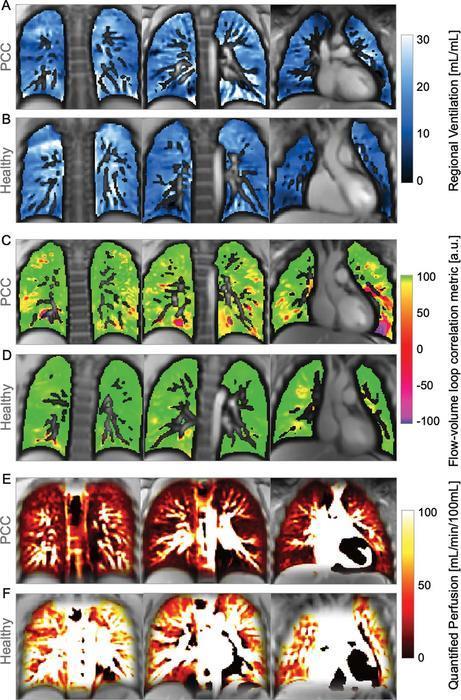
Compared to healthy controls, children and adolescents with long COVID had significantly reduced blood flow in the lungs. A reduction in blood flow patterns in organs or other areas of the body can result in a lack of sufficient oxygen and nutrients.
The most prevalent symptom of fatigue affected all but one patient with long COVID.
Biological basis
“Importantly, the severity of fatigue symptoms correlated with these blood flow changes, suggesting a possible biological basis for the patients’ ongoing symptoms,” Dr. Pöhler said.
In addition to poor blood flow, a subgroup of long COVID patients with cardiopulmonary symptoms, such as shortness of breath, also showed a reduction of air movement and reach in the lungs.
The researchers suggest that continuous monitoring of lung abnormalities in children with long COVID at various stages of the condition could help guide therapeutic interventions and monitoring strategies.
“Quantitative lung MRI establishes a potential imaging biomarker profiling and helps to enable disease severity follow-up for this complex condition in the future,” Dr. Pöhler said.







No comments yet