The drugs used to treat and prevent malaria in Mozambique are still effective, according to a genomic analysis of drug resistance markers in Plasmodium falciparum, carried out by the Barcelona Institute for Global Health (ISGlobal) and the Manhiça Health Research Center (CISM).
The results of the study, published in Communications Biology, also revealed a geographical differentiation of the parasite.
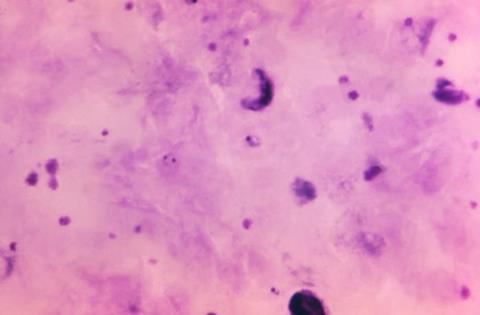
A key element in the fight against malaria is the use of antimalarial drugs to prevent or treat the disease. However, the malaria parasite P. falciparum has developed resistance to many of these drugs.
For example, resistance to artemisinin, the first-line treatment for P. falciparum malaria, is characterised by mutations in the parasite gene pfkelch13. Resistance to sulfadoxine-pyrimethamine (SP), used to prevent malaria in pregnancy and infancy, is mostly associated with three mutations in the pfdhps gene and two mutations in the pfdhfr gene.
Drug resistance markers
Monitoring the presence and spread of these drug resistance markers is therefore crucial to inform malaria control programmes and ensure that the drugs used remain effective.
“In Mozambique, several studies have reported markers of drug resistance, but little was known about their geographical distribution,” says Alfredo Mayor, researcher at ISGlobal and CISM. This is relevant because malaria transmission in Mozambique is very heterogeneous, with a high burden in the north and very low transmission in the south.
In this study, Mayor and his team examined the geographical distribution of antimalarial drug resistance markers in the country over several years. To do this, they used cutting-edge techniques to sequence 2,251 P. falciparum samples collected between 2015 and 2018 across south, central and north Mozambique.
North-south divide
Genomic analysis revealed no evidence of markers linked to artemisinin resistance, and a very low prevalence of resistance markers to chloroquine or piperaquine (which is used in combination with artemisinin).
In contrast, the frequency of SP resistance markers was very high: quintuple mutants (carrying the three mutations in pfdhps mutations plus the two in pfdhfr) increased from 80% in 2015 to 89% in 2018, and increased from north to south of the country. This spatial gradient was also accompanied by a reduction in the number of genetically distinct parasites infecting an individual, reflecting the lower intensity of malaria transmission in the south.
Another mutation, also linked to SP resistance, was only detected in the north of the country (Cabo Delgado) at a frequency of 17% and never in combination with the two mutations in the pfdhr gene.
“We see a regional differentiation of the parasite, which could be due to several factors, including geographical distance and differences in the use and coverage of antimalarial interventions,” says Simone Boene, co-first author of the study together with Clemente da Silva.
Public health implications
The findings have several public health implications for Mozambique. First, that artemisinin remains effective for treating P. falciparum malaria. Second, that piperaquine can be used in artemisinin combination therapies (ACT). Third, despite the high frequency of quintuple mutants, there is no evidence of reduced chemopreventive efficacy of SP.
Another mutation in pfdhps, known to reduce the effect of the drug in infants and pregnant women, was detected in only 0.2% of analysed samples, supporting the continued use of SP to prevent malaria in pregnant women (IPTp). However, the authors warn that these resistance markers need to be closely monitored, given the rapid rise of artemisinin and piperaquine resistance in southeast Asia.
“These results provide baseline data for studying the evolution of P. falciparum parasites in response to changing national malaria treatment guidelines,” says da Silva. The authors highlight the need to integrate molecular surveillance systems with drug efficacy studies to track the emergence and spread of drug-resistant parasites.
Topics
- Alfredo Mayor
- Antimicrobial Resistance
- artemisinin
- Barcelona Institute for Global Health
- chloroquine
- Clemente da Silva
- Infectious Disease
- malaria
- Manhiça Health Research Center
- Middle East & Africa
- Mozambique
- One Health
- Parasites
- piperaquine
- Plasmodium falciparum
- Research News
- Simone Boene
- sulfadoxine-pyrimethamine
- UK & Rest of Europe







No comments yet