MIS-C is a serious inflammatory shock that affects children. It can occur several weeks after a COVID infection and can be life-threatening. Until now, however, the precise cause of the condition was unknown.
Researchers at Charité – Universitätsmedizin Berlin and the German Rheumatology Research Center (DRFZ), an institute of the Leibniz Association, have identified that reactivation of a pre-existing, dormant infection with the Epstein-Barr virus triggers an excessive inflammatory response. The researchers have detailed their findings in an article in Nature. These insights open the door to new treatment methods, potentially not limited to MIS-C.
READ MORE: Genes combined with immune response to Epstein-Barr virus increase MS risk
READ MORE: ‘Failed drug’ could offer new approach to Epstein-Barr virus and resulting diseases
The majority of children who contract COVID experience mild symptoms. In very rare cases, however, young patients can become seriously ill. Even if the child experiences only mild symptoms or is asymptomatic, several weeks after an acute infection, their immune system can go haywire and attack their organs.
In such instances, children can develop cardiac insufficiency, skin rashes and a high fever. Their immune system must be stabilized through hospital-based care to avert organ failure. In around half of these cases, pediatric patients are even admitted to intensive care. The cause of this condition, known as Multisystem Inflammatory Syndrome in Children (MIS-C), has not been conclusively determined until now.
Waking up from dormancy
“Discussions around the potential causes of MIS-C included the coronavirus surviving in the body, for example, or the immune system turning on itself,” says Prof. Tilmann Kallinich, Head of the Division of Rheumatology in the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine at Charité, and one of the study’s two lead authors.
“We’ve now found indications, however, that a resurgence of a second pathogen – the Epstein-Barr virus – is responsible for the inflammatory shock. Put simply, it wakes up from a dormant state because the COVID infection has thrown the child’s immune system in such disarray that it becomes unable to keep the dormant infection in check.”
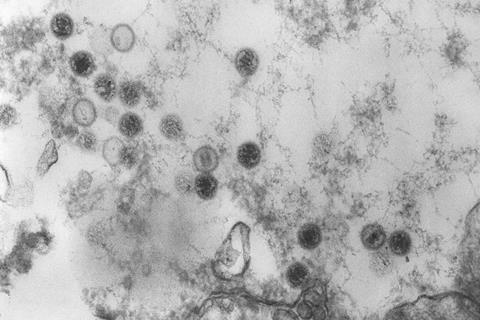
The Epstein-Barr virus (EBV) is the pathogen that causes glandular fever (also known as infectious mononucleosis, or “mono” for short), which is accompanied by flu-like symptoms and from which people sometimes take weeks to recover. For the most part, however, this infection goes unnoticed, as roughly 90% of people will contract the pathogen at some point in their life.
Flare-ups years later
“Following an acute infection, however, the virus is not removed from the body,” explains Tilmann Kallinich, who also leads a liaison working group at the DRFZ. “The Epstein-Barr virus settles in different cells in the body, thereby escaping the immune defenses. Consequently, it remains in an infected person’s body for the rest of their life. The virus can flare up again years after the initial infection, including when immune systems are weakened.”
The research team has now identified a flare-up of an Epstein-Barr viral infection in children with MIS-C. The study examined 145 children aged between 2 and 18 years old who had been treated for MIS-C at the Children’s Hospital at Charité or at hospitals in Lyon (France), Naples (Italy), Ankara (Türkiye) and Santiago (Chile).
By way of comparison, the study also examined 105 children who went through a COVID infection without developing MIS-C. The researchers found traces of the Epstein-Barr virus in the blood of children with MIS-C, along with antibodies and high levels of specific immune cells against the virus – indicating that the body is actively fighting the pathogen.
Reactivation trigger
“We’ve also determined that, although the immune cells set out to fight off the Epstein-Barr virus, they’re effectively fighting with blunt weapons,” explains Dr. Mir-Farzin Mashreghi, Deputy Scientific Director of the DRFZ and a researcher at the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine at Charité. Dr. Mashreghi spearheaded the study alongside Prof. Kallinich. “The immune cells are no longer able to kill off body cells infected with EBV.”
The researchers were able to attribute this inability to unusually high levels of a messenger substance called transforming growth factor beta (TGFβ), which the child’s body produces as a result of the COVID infection. TGFβ is a molecule that suppresses inflammation, inhibits the function of immune cells and thus curbs their ability to attack the Epstein-Barr virus.
“In some children, COVID triggers a rapidly intensifying system: the messenger substance TGFβ prevents immune cells from keeping the Epstein-Barr virus in check, which enables the virus to proliferate again,” says Dr. Mashreghi, summarizing the new insights into the causes of MIS-C. “In response, the body produces more immune cells to fight the virus, but these immune cells are still not functional. This culminates in an extreme inflammatory response that damages organs and can, potentially, be fatal.”
Potential treatment for MIS-C and long COVID
The inflammatory cascade can be interrupted effectively with hospital medication, and the vast majority of children recover from MIS-C. To date, anti-inflammatory drugs such as immunoglobulins and cortisone-based preparations have been deployed to treat MIS-C.
“Our insights suggest that an early and targeted blockade of TGFβ could help to treat MIS-C,” summarizes Kallinich. “However, these new insights could also be relevant for the treatment of other COVID-related conditions.”
There are indications, for example, that reactivation of dormant viruses could play a role in long COVID. “There could be parallels with the processes at work in MIS-C, which would make TGFβ inhibitors potential candidates for a treatment for long COVID,” says Mashreghi. “Furthermore, we know that high TGFβ levels in adults correlate with severe cases of COVID-19. We therefore suspect that a TGFβ blockade could have a positive influence on the course of COVID-19.” Further studies are now required to ascertain whether TGFβ inhibitors prove effective treatments for COVID-related illnesses.







No comments yet