Aspergillus fumigatus strains that infect humans have a significantly altered metabolism compared to other strains in the environment. At the same time, infection with the fungus leads to an apparent change in the human lung microbiome.
Researchers at the Leibniz Institute for Natural Product Research and Infection Biology (Leibniz-HKI) in Jena, Germany, came to this conclusion after using machine learning models to analyze genome data from about 250 fungal strains and lung microbiome data from 40 patients.
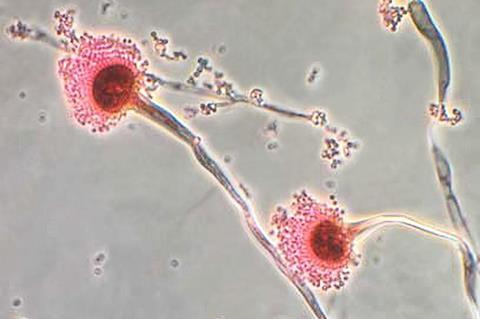
The fungus Aspergillus fumigatus is widely distributed in the environment, where it performs important ecological functions. At the same time, it is an opportunistic pathogen of humans. This means that it can infect people with a weakened immune system and cause life-threatening diseases like aspergillosis. Treatment is difficult due to the limited number of drugs available for fungal infections.
Variations in genetics
However, as researchers at Leibniz-HKI have discovered, fungal strains found in the environment and clinical strains from patient samples differ significantly. In a previous study, the team already found that the genetic information of about 250 Aspergillus fumigatus strains of different origins matched only by about 70 percent. By comparison, the genetic information of humans and pigs is about 95 percent identical.
“In the current study, we focused on what impact these genomic differences have on fungal metabolism in the presence of a complex lung microbiome,” said study leader Gianni Panagiotou. He heads the Microbiome Dynamics department at Leibniz-HKI and holds a professorship at Friedrich Schiller University in Jena, Germany.
“Understanding what might drive fungal growth, and thus survival, of A. fumigatus in different habitats might advance the development of prophylactic or therapeutic strategies to control the fungal pathogen levels.”
Metabolic differences
The research team developed computer models that predict metabolic reactions and products for the 250 different strains, based on the genome data and current knowledge of metabolic pathways. “In doing so, we found that the clinical strains differ significantly from the environmental strains, especially in the area of amino acid synthesis,” says Mohammad Mirhakkak, one of the two lead authors.
Mirhakkak and his co-first author Xiuqiang Chen then used the model they developed to study samples from 40 patients with cystic fibrosis before and after confirmed Aspergillus fumigatus infection.
Using metagenome data from the samples, they were able to decipher the composition of the lung microbiome before and after infection. In other words, they determined microorganisms that live in each patient’s lungs.
“We used these data to feed our model and found that Aspergillus fumigatus appears to shape the lung microbiome to its advantage,” Chen explains.
Surviving knockouts
Even when the researchers simulated so-called knockouts - strains of fungi that are not viable on their own because certain metabolic pathways have been turned off - they survived thanks to the help of the lung microbiome. At least in the computer simulation, other microorganisms then took over the production of vital metabolites.
“Our results show that when developing new drugs, we need to keep in mind, on the one hand, the enormous variability of the metabolism of Aspergillus fumigatus, and on the other hand, that we also need to keep the entire microbiome in mind,” Panagiotou said.
The study was funded by the German Research Foundation as part of the Collaborative Research Center (Transregio) FungiNet and the Cluster of Excellence Balance of the Microverse, and by the German Federal Ministry of Education and Research.







No comments yet