Preclinical trials have shown that zika virus can inhibit the spread of prostate cancer, suggesting its potential use in treating the disease. However, a new study by researchers at the State University of Campinas (UNICAMP) in São Paulo State, Brazil, shows that zika can trigger a persistent inflammatory process in healthy epithelial cells and damage the male reproductive system.
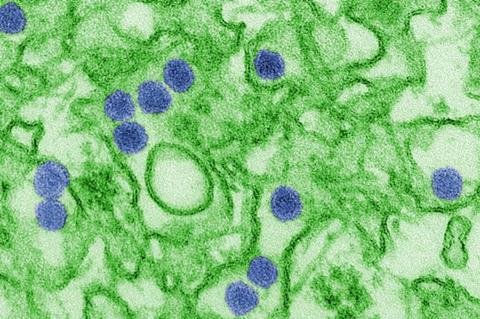
The researchers analyzed the effects of the virus on tumour cells and healthy cells, reporting their findings in an article published in the Journal of Proteome Research.
After the 2015 zika outbreak in Brazil, a group at UNICAMP led by Professor Rodrigo Ramos Catharino began studying zika’s effects on biofluids such as saliva, serum and semen, as well as investigating whether prostate cells could act as a viral reservoir. In 2019, they discovered that inactivated zika viruses could be used to treat not only nerve tumors, such as glioblastoma, but also prostate cancer.
Although other studies had suggested that zika easily replicates in healthy prostate epithelial cells and human prostate adenocarcinoma cells, more research was needed to analyze the mechanisms of persistent infection by the virus and its consequences for the metabolism of cells.
Two phenotypes
“We set out to compare the two phenotypes, tumoral and normal, since both are present in prostate cancer, and we needed to know how harmful infection could be,” said Jeany Delafiori, first author of the article and currently a research assistant at the European Laboratory of Molecular Biology (EMBL) in Germany.
The study, which was supported by FAPESP, was the first to use an in vitro prostate cell model in a metabolomic assay – an analysis of all products of the metabolism of infection by zika.
Infected normal prostate epithelial cells (PNT1a) and adenocarcinoma cells (PC-3) were extracted, ionized and infused into a high-resolution mass spectrometer. A statistical analysis of the data was based on exposure for five, ten and 15 days after infection.
“We observed the effects on the PC-3 cells for the first five days and checked our findings against those of previous studies that pointed to anticancer action,” Delafiori said, noting especially the antiproliferative lipidic alterations. More of these cells died as exposure progressed. “The results could serve as the basis for treatment of prostate cancer,” Catharino said.
Metabolomic alterations
In the case of PNT1a cells, infection by zika led to noteworthy metabolomic alterations, especially regarding glycerolipids, fatty acids and acylcarnitines during the longest period of infection.
According to the authors, these effects could be linked to an increase in oxidative stress metabolites associated with carcinogenesis, such as dityrosine, aminotyrosine and hydroxyguanosine, so that long-term treatment itself could cause a recurrence of prostate cancer, and prolonged infection would contribute to its malignancy by subjecting cells to even more stress.
Having shown that zika virus can act on prostate cancer cells, the researchers must now conduct more studies to investigate its effects on similar cells in order to confirm the discovery and analyze metabolic and replication-related factors.
Although the finding that zika can have carcinogenic effects on healthy prostate epithelial cells could have been considered a setback, the researchers concluded that it was positive.
“All these questions were relevant in the initial stage of our research, so that future patients who opt for treatment of this kind in future have all the necessary information,” Catharino said.







No comments yet