More than half of us are carriers of chronic herpesvirus infections. But even though the herpesvirus can infect our nerve cells, it rarely causes serious infection of the brain. Researchers from Aarhus University have now discovered a key element of the explanation.
The researchers have discovered a previously unknown defence mechanism in the body that is the reason why herpes infection causes a serious and potentially fatal brain inflammation in only one out of 250,000 cases. The study has recently been published in the scientific journal Nature.
READ MORE: Has a viral contribution to Alzheimer’s disease been in front of our noses this whole time?
READ MORE: Study reveals how the immune system fights to keep herpes at bay
“The study has exciting perspectives because it gives us a better understanding of how the brain defends itself against viral infections,” says Professor Søren Riis Paludan from the Department of Biomedicine at Aarhus University. He is the article’s last author, a Lundbeck Foundation Professor and centre director of the Excellence Centre CiViA.
“We’ve discovered how our body prevents herpesvirus from entering into the brain, even though 50-80% of us are chronically infected with this particular virus. The idea behind CiViA is that we want to understand how the body fights infections without harming itself at the same time. The mechanism we’ve found doesn’t cause inflammatory reactions,” he says.
Protective gene
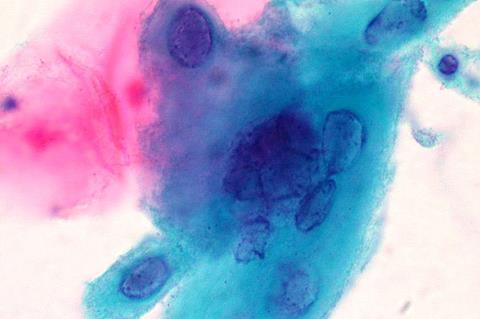
The answer lies in the protective TMEFF1 gene. Many years of experimenting with the genome-wide CRISPR screening technology and development of mice that lacked the critical gene have finally convinced the researchers that TMEFF1 produces a protein that prevents herpesvirus from entering into nerve cells.
The study in Nature is accompanied by another article describing two patients with brain inflammation caused by herpesvirus infection, called herpes encephalitic. In a collaborative study led by researchers in New York, the research group in Aarhus discovered that two children who developed herpes encephalitis were carrying a genetic defect that disabled the protective TMEFF1 gene.
“The new study is groundbreaking because it updates the basic understanding of immunity against viral infections,” explains Søren Riis Paludan.
“This is interesting for immunologists because it illustrates that there are still many immunological mechanisms in the brain that we don’t know about. “The study is also relevant for neuroscience because it sheds light on how the brain, so to say, prevents unwanted visitors from intruding without causing harm to the brain itself, i.e. the neuronal cells,” he says.
Better understanding of Alzheimer’s
Søren Riis Paludan hopes that the study is the first step towards revealing a completely new range of brain defence mechanisms. One of the tracks that the researchers will now investigate is what the discovery may mean for the development of dementia.
Research has already demonstrated a correlation between infection with herpesviruses and later development of Alzheimer’s disease.
“Perhaps our discovery of a new antiviral mechanism in the brain can help to clarify whether individual differences in this particular mechanism or similar mechanisms can give the virus access to the brain and accelerate neurodegenerative processes,” says Søren Riis Paludan.






No comments yet