A team led by investigators at Massachusetts General Hospital (MGH) has determined that the SARS-CoV-2 Omicron BA.2 subvariant is less severe than the previous Delta variant and less severe to an even greater extent than the original Omicron variant.
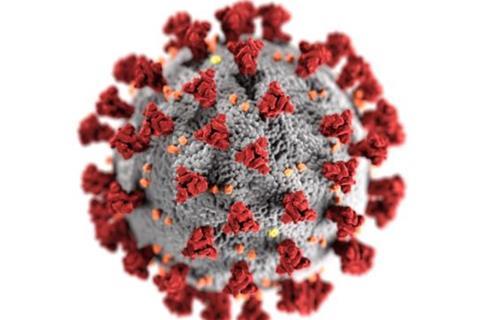
Following a recent study that represents the largest to date to examine the severity of the SARS-CoV-2 Omicron BA.2 subvariant, the strain making a re-emergence this autumn, this pattern revealed in the JAMA Network Open study suggests that the severity of SARS-Cov-2 may be diminishing.
To provide an accurate assessment of the severity of SARS-Cov-2 variants above and beyond previous studies, the researchers used a method called entropy balancing to account for potential confounding factors such as prior infections, vaccinations, treatments, and comorbidities.
The team applied this method to data leveraged from the Mass General Brigham’s electronic health record system that’s linked to a COVID-19 vaccine registry.
Of 102,315 confirmed COVID-19 cases from March 3, 2020 to June 20, 2022, there were 20,770 labeled as Delta variants, 52,605 labeled as Omicron B.1.1.529 variants (the original Omicron variant), and 28,940 labeled as Omicron BA.2 subvariants.
Mortality rates were 0.7% for Delta, 0.4% for the original Omicron variant, and 0.3% for Omicron BA.2. After adjustments, the odds of death were more than 2 times higher for the Delta and the original Omicron variant compared with Omicron BA.2. Patients with Delta and original Omicron variants were also more likely to need hospitalisations, invasive ventilation, and intensive care admissions.
“While the SARS-CoV-2 virus always has the potential to mutate to a more deadly form, when you look at the recent trajectory of Delta, Omicron BA.1, to Omicron BA.2, the virus seems to be getting intrinsically less severe. Hopefully this trend will continue,” said lead author Zachary Strasser, MD, MBA, an academic physician in the Laboratory of Computer Science at MGH and an Instructor of Medicine at Harvard Medical School.
“We can continue to use our analytics system and method to assess many other questions such as which vaccinations have the most impact on preventing long COVID, or whether certain treatments reduce the likelihood of long COVID.
Additional co-authors include Noah Greifer, PhD, Aboozar Hadavand, PhD, Shawn N. Murphy, MD, PhD, and Hossein Estiri, PhD.
This work was supported in part by the National Institute of Allergy and Infectious Disease and the National Human Genome Research Institute.







No comments yet