An innovative, safer, simpler, patient-friendly oral medicine to treat visceral leishmaniasis has entered Phase II clinical development in a trial conducted in Ethiopia by the not-for-profit research organization Drugs for Neglected Diseases initiative (DNDi) and its partners.
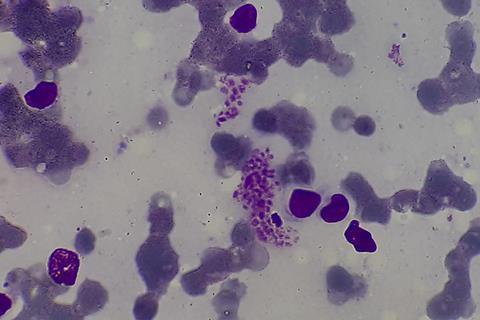
Also known as kala-azar, visceral leishmaniasis is the world’s deadliest parasitic killer after malaria.
It causes fever, weight loss, spleen and liver enlargement, and, if not treated, death. Kala-azar is transmitted by the bite of infected sandflies and is endemic in 80 countries, mainly in Eastern Africa, South Asia, and Latin America.
One billion people are at risk globally and Eastern Africa has currently the highest number of cases. As for other vector-borne diseases, climate change is changing the epidemiology of leishmaniasis and could lead to its expansion to new areas. An estimated 50,000 to 90,000 new cases occur worldwide annually, and half are children under 15.
Daily injections
In Africa, the current treatment for visceral leishmaniasis includes painful injections given at hospital daily for 17 days, a treatment that may also present rare but life-threatening side effects, including to the heart, liver, and pancreas. In contrast, the new molecule under study in Ethiopia, called LXE408, is administered in the form of oral pills and is expected to be safer than the current treatment.
”This is very significant that Ethiopia, an endemic country, is conducting a Phase II clinical trial on a new chemical entity — a novel molecule with the potential to safely and effectively treat visceral leishmaniasis,” said Dr Eleni Ayele, co-Principal Investigator of the clinical trial at the Leishmaniasis Research and Treatment Center (LRTC), University of Gondar, Ethiopia.
”Current treatment options in Ethiopia have severe limitations: they are potentially toxic, necessitate injections and cold-chain supplies, and require our patients to travel to faraway hospitals and be hospitalized for long periods.
“Our hope is that this new oral treatment will be efficacious and less toxic and can be given to patients at the primary healthcare level, close to their homes. This would help them access treatment earlier, which could significantly decrease morbidity and transmission. If the trial is successful, it could go a long way toward enabling the sustainable elimination of this terrible disease.”
Phase II testing
The molecule is tested alongside the standard of care in Ethiopia (a combination of daily injections of sodium stibogluconate and paromomycin administered for 17 days); 52 adults from 18 to 44 years will join the study.
A similar Phase II trial to test LXE408 alongside the standard of care is also being conducted in India. Patients in Eastern Africa and South Asia may respond differently to treatments, which is one of the reasons why finding new medicines is particularly difficult and why studies on both continents are necessary.
”We are moving towards a new generation of treatments for leishmaniasis. Finding new treatments is key if we want to sustainably eliminate visceral leishmaniasis in all parts of the world, including in African countries where the burden remains high. We need medical innovation,” said Dr Fabiana Alves, Director of Leishmaniasis programme at DNDi. ”We hope this new clinical trial will contribute to deliver better, patient-friendly, effective medicines that are accessible to everyone, with no exception.”
Affordable vaccine
LXE408 was initially discovered by Novartis. DNDi and Novartis initiated a collaboration and licence agreement in early 2020 to jointly develop LXE408. Novartis was responsible for completing pre-clinical development and a Phase I study, is in charge of chemical manufacturing and control, will drive regulatory submissions, and – if trial results are positive and if the new treatment is approved for market use – has committed to distributing the drug on an affordable basis worldwide, with a focus on maximizing access in endemic countries.
Discovery of LXE408 and preparatory work to advance LXE408 to clinical evaluation in kala-azar patients were financially supported by Wellcome. The clinical trial in Ethiopia is financially supported by the European and Developing Countries Clinical Trials Partnership (EDCTP), as part of the VL-INNO project, bringing together a wide range of partners.
Eastern African countries are currently laying out plans to sustainably eliminate visceral leishmaniasis, a disease that can potentially see a resurgence due to climate and environmental changes. Achieving and sustaining elimination also hinges on the development of better treatments. If proven to be effective, LXE408 could therefore contribute significantly to these elimination goals.
Drive to eliminate
”Visceral leishmaniasis is a severe and potentially fatal disease that primarily impacts vulnerable groups such as children. We urgently need to eliminate it, which would greatly help lift affected communities out of poverty,” said Dr Saurabh Jain, Scientist and Focal Point for Visceral Leishmaniasis at the World Health Organization (WHO). ”One of the targets in our roadmap for neglected tropical diseases is the elimination of visceral leishmaniasis as a public health problem by 2030. Developing better diagnostics and treatments is one of the critical actions to reach and sustain that objective.”
Financial and technical support for the study is provided by the European and Developing Countries Clinical Trials Partnership (EDCTP2) through grant RIA2020I-3290; Norway-Norwegian Agency for Development Cooperation (Norad), Norwegian Ministry of Foreign Affairs, as part of Norway’s in-kind contribution to EDCTP2; Germany’s Federal Ministry of Education and Research (BMBF) through KfW; Médecins Sans Frontières International; the Swiss Agency for Development and Cooperation (SDC); UK International Development; and other private foundations and individuals.






No comments yet