Antibacterial drugs are important for treating infections. But increasingly, bacterial resistance to current drugs — so they don’t work well, or even at all — means new ones are urgently needed.
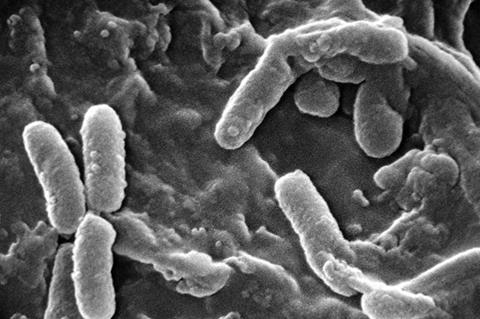
Building on previous work, researchers in ACS Infectious Diseases have demonstrated a potential antibacterial treatment from a modified darobactin, a compound sourced originally from a bacterium. The team reports proof-of-concept animal trials on infections caused by bacteria, including E. coli, that are known to develop drug resistance.
This study was published during the World Health Organization’s World Antimicrobial Resistance (AMR) Awareness Week from November 18 to 24.
Updated list
Earlier in 2024, the World Health Organization updated its list of bacterial pathogens that can develop resistance to antibiotics to include Acinetobacter baumannii, Pseudomonas aeruginosa and E. coli, among others. Despite the need for new antibiotics that target these priority pathogens, scientists don’t have many candidates.
One potential resistance-breaking compound is called darobactin, a naturally produced antibiotic discovered in a bacterium. Darobactin binds to an essential protein in cells of different bacteria and eventually causes their death. Previously, Rolf Müller, Jennifer Herrmann and colleagues showed that genetically engineered versions of darobactin have antibacterial activity. Specifically, one of these non-natural, biosynthetic darobactins (called D22) inhibited A. baumannii growth in lab assays.
READ MORE: Genetic analysis of bacteria from humans and animals paves the way for new active ingredients
READ MORE: Researchers identify new tools for anti-Acinetobacter drug development and AMR preparedness
For this new study, a larger team led by Müller and Herrmann tested the engineered D22 compound against several priority bacterial infections in animals. First, in zebrafish embryos, D22 treatment cleared A. baumannii infection as effectively as ciprofloxacin, a broad-spectrum antibiotic used for complicated infections.
Series of trials
Then the team conducted a series of efficacy and dosing trials with mice:
- Best delivery method: Observations indicated that administering D22 as an injection was more effective than via mouth.
- Efficacy against P. aeruginosa: Repeated doses of D22 substantially limited P. aeruginosa bacterial growth in mice (thigh tissue infection) but didn’t fully clear the infection.
- Multi-dose experiments against E. coli: Administering D22 four times in 25 hours fully cleared E. coli in a severe infection model of peritonitis (abdomen infection). Activity was also observed for single doses. Twice-daily D22 injections over three days significantly reduced bacterial presence in a complicated E. coli urinary tract infection, although not as low as the antibiotic gentamicin, which reduced bacterial loads below detection.
These results show that D22 can inhibit critical infections and highlights the compound’s promise for further development toward future clinical trials as “an innovative solution to fight antimicrobial resistance,” say the researchers.
The authors acknowledge funding from the Helmholtz Impuls- und Vernetzungsfonds (Impulse and Networking Fund). Some of the authors are employees of Evotec, a biotechnology company involved in drug discovery and development.
The paper’s abstract will be available on Nov. 20 at 8 a.m. Eastern time here: http://pubs.acs.org/doi/abs/10.1021/acsinfecdis.4c00687







No comments yet