Prolacta Bioscience® has announced that the peer-reviewed journal Cell Host & Microbe has published its study demonstrating that a synbiotic comprising human milk sugars, called human milk oligosaccharides (HMOs), and a strain of bacteria found in the gut of nursing infants, Bifidobacterium infantis (B. infantis), can safely and predictably control the gut microbiome in adults.

This is the first time that scientists have been able to modulate the adult gut microbiome with significant precision, the company said.
The prospect of ’precision microbiome engineering’ may open the door to the development of live biotherapeutic products that effectively reconstitute a damaged or out-of-balance microbiome, as is the case in numerous infectious, autoimmune, and metabolic disorders.
Engineering the gut microbiome
For the last decade, researchers have been working on methods to engineer the gut microbiome in patients, drawing inspiration from the success of faecal microbiome transplants for treating Clostridioides difficile (C. diff) infections.
“While some of these attempts have been clinically successful, they have been quite crude and undefined, lacking in precision and reproducibility,” said Greg McKenzie, vice president of product innovation at Prolacta.
Changing ecology
In the current study “Precision Modulation of Dysbiotic Adult Microbiomes With a Human Milk-Derived Synbiotic Reshapes Gut Microbial Composition and Metabolites,” researchers from Prolacta, MD Anderson Cancer Center, and the University of Texas Southwestern Medical Center observed:
- HMOs support engraftment of B. infantis in healthy adults with a median observed abundance of 45.9% and up to 81% relative abundance in antibiotic-treated adults; no serious adverse events were observed.
- Microbiome structure and gut metabolite levels were altered in engrafted subjects. When B. infantis was present, other members of the microbiome that are not directly influenced by HMOs changed in a reproducible manner. One notable example was a microbe called Veillonella that feeds on molecules produced by B. infantis and subsequently generates metabolites that are beneficial to human health.
Downstream effects
“These findings are incredibly exciting, as we are starting to do ecology in the human microbiome,” said Julie Button, Ph.D., director, non-clinical development at Prolacta. “The reproducibility of cross-feeding Veillonella is really striking, as this magnitude of downstream effects are normally seen only when treating patients with antibiotics.”
“We expect that this human milk-based synbiotic will have the power to repair the microbiome of sick patients using the same biology that establishes a healthy microbiome in infants,” said Scott Elster, CEO of Prolacta. “We plan to demonstrate what is essentially `Nature’s Microbiome Starter Kit’ in extremely fragile stem cell transplant patients in a Phase 2a clinical trial starting in Q3 2023.”
Power of HMOs
Human breast milk contains high concentrations of a collection of approximately 200 structurally diverse sugars called HMOs. Unlike the nutritional components of breast milk, HMOs are not metabolized as an energy source by the infant.
Instead, HMOs serve to guide the growth of appropriate bacteria in the gut, which helps to train the infant’s immune system. In this way, HMOs support protective responses such as suppression of inflammation and improved intestinal barrier function to minimize infections.
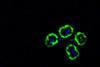
One species of ‘good’ bacteria in the infant gut that is known to influence these protective responses is B. infantis, which is unique in its ability to utilize the HMOs in human breast milk. After infants are weaned from human milk, B. infantis levels decline into adulthood.
Study details
This unblinded clinical study enrolled 56 healthy adult subjects. A control group completed a five-day course of antibiotics (known to disrupt gut bacteria) with no other intervention. A second group received the same course of antibiotics along with B. infantis for 14 days, and a third group additionally received HMOs for 28 days.
Stool and blood were collected at set intervals for a total of 35 days. This trial built upon prior research from the same investigators published in 2022 in which it was observed that dosing with a synbiotic of HMOs and B. infantis led to controllable, HMO-dependent engraftment of B. infantis in healthy adult subjects.
This fall, Prolacta will initiate a Phase 2a Investigational New Drug (IND) trial to evaluate the human milk-based synbiotic in patients undergoing stem cell transplant for blood cancers. Patients undergoing stem cell transplant often have disruptions in their gut microbiome, including an increase in numbers of potentially disease-causing species of bacteria and an overall loss of diversity.
This leaves patients prone to opportunistic infections and graft-versus-host disease (GVHD), which can result in multi-organ attack and mortality. The study will measure how well the synbiotic drives redevelopment of a healthy microbiome, like it does naturally in the newborn gut.






No comments yet