In work published today in Nature, researchers’ structural insights helped reveal a weak spot in malaria’s plan of attack which could help guide vaccine design. Contributors hailed from Fred Hutch, the Scripps Research Institute, the University of Copenhagen and The University of Texas Health Science Center at San Antonio, as well as the Tanga Research Centre, the Infectious Disease Research Collaboration in Uganda, and the University of California, San Francisco.
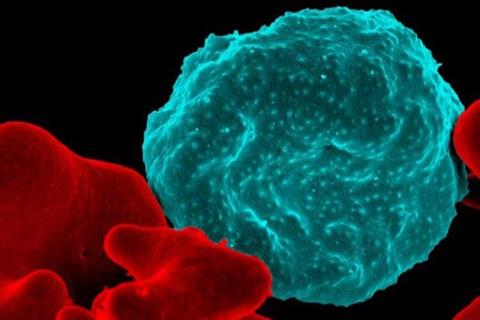
Antibodies are immune proteins that our bodies produce to help fight off infection. Where they recognize and bind a pathogen — and how — can give important clues to the microbe’s vulnerabilities. Fred Hutch Cancer Center structural biologists Marie Pancera, PhD and Nicholas Hurlburt, PhD, understand how subtleties of antibody-target interaction can guide development of better treatments and vaccines.
“When you look at the structures of antibodies and their targets, you learn how they interact and where the antibody binds,” Pancera said. “The visualization of ‘sites of vulnerability’ gives you information you can use to inform vaccine design.”
These insights can reveal where investigators should focus vaccine efforts and how to modify microbial structures to improve protective responses to vaccines. Pancera hopes to provide these insights for antibodies that scientists can use to help prevent or treat diseases, like malaria and HIV, that remain health burdens around the world.
Structural insights
Most recently, she and Hurlburt, a staff scientist on Pancera’s team, contributed structural insights that helped an international team of investigators show that broadly inhibitory antibodies can target a key part of the protein that malarial parasites use to snag infected red blood cells on blood vessels.
READ MORE: Maternal antibodies interfere with malaria vaccine responses
“The idea would be that we can use this structural information about how the antibody binds a specific epitope [target] to then try to computationally design [a vaccine] that would elicit this sort of antibody response,” Hurlburt said.
His work could also provide insights that could guide the development of monoclonal antibodies that could help reduce disease severity, he said.
If our bodies mount a protective antibody against one variant, the parasite can sidestep them by expressing a different version. But some antibodies can block many versions of their target. Called broadly neutralizing antibodies, they’re what scientists hope to induce with a vaccine. Severe disease mostly occurs in children under five, suggesting that a broadly protective response can develop over time, Hurlburt said.
Identified two broadly neutralizing antibodies
The teams of co-senior authors Evelien Bunnik, PhD, at UT Health San Antonio, and Thomas Lavstsen, PhD, at the University of Copenhagen had identified two broadly neutralizing antibodies against PfEMP1. Though each was isolated from a different individual, they exhibited similar properties when the collaborators tested their ability to interfere with PfEMP1’s ability to interact with the molecule it uses as a toehold on blood vessel walls. And in lab dish-based models of malaria infection, both antibodies prevented infected red blood cells from sticking to blood vessel walls.
Hurlburt used X-ray crystallography to visualize how an arm of one of the broadly neutralizing antibodies interacts with a key segment of PfEMP1. He showed that it docks at the region of PfEMP1 that grabs the toehold molecule on blood vessels walls.
“This informed what direction to go in,” Hurlburt said.
Hurlburt and collaborators’ further work, including the use of cutting-edge cryo-electron microscopy, showed that both of the broadly neutralizing antibodies zero in on the same critical section of PfEMP1, a section that is known to be made up of a consistent (or “conserved”) set of amino acids in different versions of PfEMP1.
Antibody binds whole class of proteins
Hurlburt also used an optical biosensing technology called bio-layer interferometry to test how well the two antibodies bind different versions of PfEMP1.
“I showed that the antibody doesn’t just bind one PfEMP1 well, it binds the whole class [of proteins] very well,” he said.
The structural work helps shed light on both the pathogen and the immune system, Hurlburt said.
“We found that both broadly neutralizing antibodies target a very conserved site that’s necessary for severe malaria,” Hurlburt said. “But they do so in different manners.”
This suggests that vaccine developers may have more than one route open to them as they map out improvements more likely to generate a protective response.
Topics
- antibody
- broadly neutralizing antibodies
- Evelien Bunnik
- Fred Hutch
- malaria
- Marie Pancera
- Middle East & Africa
- Nicholas Hurlburt
- One Health
- Parasites
- PfEMP1
- PfEMP1 proteins
- Research News
- Scripps Research Institute
- Tanga Research Centre
- the Infectious Disease Research Collaboration in Uganda
- Thomas Lavstsen
- UK & Rest of Europe
- University of California, San Francisco
- University of Copenhagen
- University of Texas Health Science Center
- USA & Canada
- Vaccinology







No comments yet