Twenty-six U.S. transplant centers collaborated in an HIV-to-HIV kidney transplant study published by The New England Journal of Medicine (NEJM). The article, Safety of Kidney Transplantation from Donors with HIV, details findings supporting HIV-to-HIV kidney transplants as safe and just as effective as those using organs from donors without HIV.
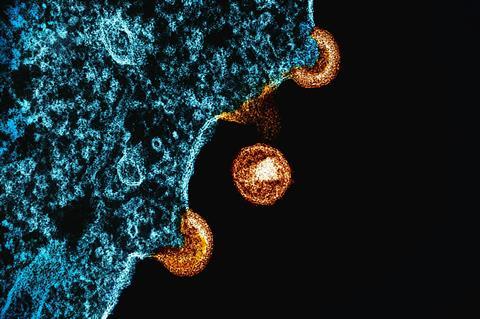
Human immunodeficiency virus, commonly known as HIV, attacks cells in the body that fight infection and there is currently no known cure. In the U.S.,1.2 million people are living with HIV. According to the National Institute of Allergy and Infectious Disease, 20 people die daily while awaiting a transplant, including those with HIV, who may have a higher likelihood than HIV-negative individuals of developing end-stage kidney and liver disease.
READ MORE: Researchers pinpoint most likely source of HIV rebound infection
The HIV Organ Policy Equity (HOPE) Act, effective since 2013, legally allows organ transplants from donors with HIV to recipients with HIV within approved clinical research studies. The NEJM article provides further evidence that HIV-to-HIV kidney transplants are safe and effective, paving the way for routine clinical application. Public comments on the proposed rule, Organ Procurement and Transplantation: Implementation of the HOPE Act, are under review by the U.S. Department of Health and Human Services. If enacted, HIV-to-HIV kidney transplants will be authorized as a standard of care clinical procedure, changing status from research use only.
Transforming lives
Jonathan Hand, MD, section head of transplant infectious diseases, served as the site principal investigator at Ochsner Transplant Institute, as part of the HOPE in Action multicenter consortium, and co-lead author. In the study, Dr. Hand and fellow researchers assessed 198 kidney transplant recipients with HIV, half who received kidneys from donors living with HIV, while half received kidneys from donors without HIV. The study evaluated primary and secondary outcomes including safety events, patient survival, infection, failure of HIV treatment and organ rejection, finding comparable results between both groups.
“We are committed to transforming lives through advanced medical research and excellent patient care at Ochsner, and we are excited to offer patients in our region access to these types of research opportunities,” said Dr. Hand. “Through the HOPE Act, we know and have seen people with HIV save lives through organ donation. The results of this study again demonstrate patients with HIV have excellent outcomes after kidney transplant if the donor has HIV or is HIV negative.
”HIV-to-HIV kidney transplant as a standard of care clinical procedure means people with HIV will benefit from a broader range of available organs, improving access and reducing wait times. There are more than 100,000 people on the national transplant waiting list, and any increase in the U.S. donor pool means the waitlist becomes shorter for everyone and more lives are saved, making the study findings even more important.”
Pioneering science
Under the HOPE Act, Ochsner was able to perform its first HIV-to-HIV kidney and liver transplant in 2019, making the Ochsner Transplant Institute the first transplant center in Louisiana and the region to offer an HIV-to-HIV liver and/or kidney transplant procedure.
This pioneering science and patient care aligns with Ochsner’s mission of healthcare accessibility for all people. The Ochsner Transplant Institute is the premier transplant center in the Gulf South region, renowned for its comprehensive range of transplant programs. Offering liver, kidney, pancreas, lung, and heart transplants, Ochsner extends its expertise to pediatric and living donor programs. Since 1984, more than 8,000 life-saving transplants have been performed at the Ochsner Transplant Institute.






No comments yet