People who are infected with chlamydia can transmit these bacteria to other people during unprotected sex. The pathogens usually cause no or only mild symptoms at first, such as itching in the vagina, penis or anus. If the infection is noticed, it can be easily treated with antibiotics. If this does not happen, the bacteria can cause serious problems, including infertility and cancer.
A phenomenon is known from everyday clinical practice that can occur after successful antibiotic treatment: when people who have already been treated come to the doctor with a new chlamydia infection, they are often infected with exactly the same strains of bacteria as the previous infection.
“It is therefore reasonable to assume that the bacteria find a niche in the body where they are not yet vulnerable, that they form a permanent reservoir there and can become active again later,” says Professor Thomas Rudel, chlamydia expert and Head of the Chair of Microbiology at the Biocentre of Julius-Maximilians-Universität (JMU) Würzburg in Bavaria, Germany. This phenomenon is known as persistence. It is problematic because the chlamydia that persist in the body become increasingly resistant to antibiotics over time.
Intestinal organoids
In which niche do the bacteria persist? Experiments on mouse models have shown that chlamydia can persist in the intestines of animals. And in humans, too, the bacteria seem to make themselves at home in precisely this place. This is reported by the research groups of Thomas Rudel and Sina Bartfeld in the journal PLOS Pathogens. Professor Bartfeld worked at JMU until 2021; she now heads the Department of Medical Biotechnology at Technische Universität Berlin.
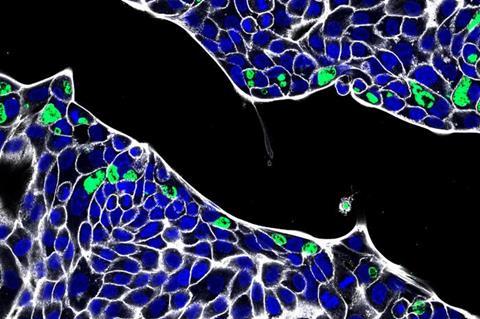
The researchers identified the intestine as a niche with the help of artificial organs in miniature format, so-called organoids. These are structures produced in the laboratory from human intestinal cells that are very similar in structure and function to the model organ.
The teams from Würzburg and Berlin tried to infect the intestinal organoids with chlamydia. They discovered that the inner cell layer of the organoids is very resistant to the bacteria: the pathogens could only penetrate there if the cell epithelium was damaged. From the blood side, however, the chlamydia were able to infect very efficiently. “In this case, we repeatedly found the persistent forms of the bacteria, which can be clearly identified with their typical shape under the electron microscope,” says JMU researcher Pargev Hovhannisyan, first author of the publication.
Clinical studies
Transferred to the human organism, this would mean that chlamydia infection with subsequent persistence can only occur with difficulty via the inner side of the intestine, but very easily via the blood. However, whether this actually happens in the human body has yet to be confirmed in clinical studies, says Thomas Rudel.
The next step for Thomas Rudel and Sina Bartfeld is to to find out whether the chlamydia select certain cell types for their persistence – no easy task, as the intestine consists of hundreds of different cell types. But perhaps it is also factors from the surrounding tissue that trigger persistence. These and other details are now to be investigated.







No comments yet