For people with autism, constipation, diarrhea, and abdominal pain often go along with the social struggles and repetitive behaviors that define the condition. This has prompted many to wonder whether gastrointestinal (GI) problems arise due to autism’s behavioral or sensory features, or whether they might instead contribute to them.

Now, scientists at University of Utah Health have added to mounting evidence showing that microbes that live in our guts influence behavior. Specifically, they found that in mice, frequent gastrointestinal distress can reduce social behaviors—an effect that persists even after GI symptoms have subsided. They also showed they could alleviate both GI symptoms and the behavioral changes they provoke by introducing specific species of bacteria into the animals’ guts.
The new study, recently published in Nature Communications, demonstrates that it is possible to impact health and behavior by manipulating the gut microbiome in a controlled way.
“I think that this is a really important step therapeutically, because now we can start to assemble a therapy with organisms that we know to be safe,” says June Round, Ph.D., a microbiologist at U of U Health, who led the research.
Gut-behavior connection
Because scientists are still trying to untangle the relationship between GI problems and autism-related behaviors, Round and her team began their study by investigating the behavioral impact of GI distress in mice. Graduate student Garrett Brown, Ph.D., studied mice with an inflammatory condition called colitis, which causes pain, diarrhea, and intestinal damage.
After several rounds of colitis, the animals’ symptoms were allowed to subside before behavioral testing. Mice that had experienced colitis moved around normally and showed no signs of anxiety or depression. However, they spent less time interacting with unfamiliar mice than mice that had not experienced colitis. “It’s not like the mice are under so much pain that they’re not doing anything,” Brown says. “So maybe it is something specific to sociability and not just that the mice feel poorly.”
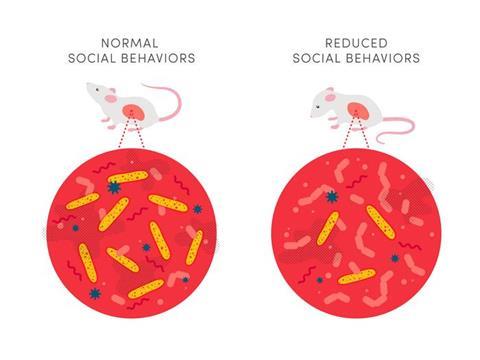
The reluctance to socialize that the researchers observed in their mice was reminiscent of the social impairments associated with autism. Since their experiments suggested that problems in the gut might drive changes to social behavior, they wondered whether the microbes there—which tend to differ between autistic and neurotypical people—might be involved in both.
Stool samples
To investigate, Brown collected stool samples from people with autism as well as from their neurotypical parents or siblings. Then he delivered the microbe-filled samples to the GI tracts of mice.
When he induced colitis in those animals, mice carrying microbes from individuals with autism had more intestinal damage and lost more weight than mice whose microbes came from neurotypical individuals. It seemed that the mix of microbes collected from neurotypical individuals had a protective effect.
The microbial community inside the human gut is so complex that the samples the team had used in their experiments could easily have included hundreds of kinds of bacteria, viruses, and fungi. Round and Brown wanted to know which of those community members protected against intestinal problems.
Potentially protective microbes
To do that, Brown compared the gut microbes from individuals with autism to those from their neurotypical family members, as well as the microbes living in the guts of mice that had been transplanted with those microbial communities. He was looking for potentially protective microbes that might be underrepresented in people with autism compared to neurotypical individuals—and he found some.
“We were able to pick out individual microbes that we thought might be playing important roles in resisting severe colitis,” explains Brown, who is now a fellow at the National Institutes of Health Clinical Center.
Two in particular stood out. Certain species of Blautia bacteria were better represented in neurotypical individuals than in their autistic family members. And among mice colonized with microbes from autistic people, a group called Bacteroides uniformis was more abundant in those whose colitis was less severe. B. uniformis is known to be underrepresented in people with irritable bowel syndrome and Crohn’s disease, suggesting a role in intestinal health.
Once the researchers had zeroed in on these groups of bacteria, Brown delivered them to mice prior to inducing colitis. Both Blautia and Bacteroides uniformis reduced intestinal problems, and the Blautia had a corresponding effect on social behavior. Animals that received the Blautia bacteria were more likely than other mice to engage with unfamiliar mice following colitis.
Toward personalized therapies
Round says the study is one of the first to identify specific organisms within the human microbiota that can ameliorate a behavioral deficit associated with GI stress. “This is an example where we are missing microbes, and missing these beneficial microbes is driving disease,” she says.
Further research will be needed to clarify whether boosting the numbers of Blautia or Bacteroides uniformis bacteria might benefit people with GI disorders, autism, or other conditions. But Round says teasing out their individual effects is an important step toward personalized microbiome-targeted therapies.
“One day, we’re going be able to quickly analyze the microbiome and say, ‘Hey, you’re missing this really important microbe. We’re going to give it back to you’,” she says.


No comments yet