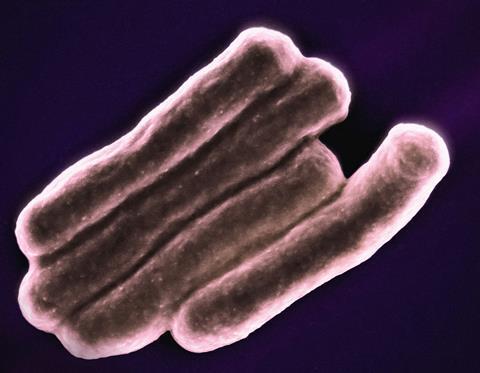
New research being presented at this year’s ESCMID Global Congress (formerly ECCMID) in Barcelona, Spain (27-30 April) has found compelling evidence that tuberculosis (TB) can have a lasting impact on the lungs of individuals who have been successfully treated for the disease.
TB survivors have smaller lungs with narrower airways and slower air flow, the analysis of data on tens of thousands of individuals from around the world found.
“This damage could have a profound effect on long-term health, reduce quality of life and affect ability to work and carry out day-to-day tasks,” says lead researcher Dr Sharenja Ratnakumar, of St George’s, University of London, London, UK. “And, with growing numbers of people being successfully treated for TB, the finding strongly indicates that post-TB lung disease is an under-recognised global challenge.”
TB can be cured with antibiotics and, worldwide, an estimated 155 million people are alive today as a result of successful diagnosis and treatment of the bacterial infection.
Increasing diagnoses
However, although significant progress has been made in combating TB in recent decades, the number of new diagnoses has increased since the COVID-19 pandemic. Some 7.5 million were diagnosed globally in 2022 – the highest number since monitoring began in 1995 and above the pre-Covid baseline of 7.1 million in 2019, according to WHO’s 2023 Global Tuberculosis Report.
The burden is highest in sub-Saharan Africa and south east Asia but even low incidence countries such as the UK are seeing diagnoses increase. According to provisional data from the UK Health Security Agency, there were 4,850 new diagnoses in England in 2023. This is above pre-Covid levels and represents a rise of more than 10% on 2022, when there were 4,380 diagnoses.
Previous research has found that between 18% and >80% of survivors will be left with lung damage that reduces their quality of life and life expectancy but data on the size and type of respiratory impairment is scarce. To find out more, Dr Ratnakumar and colleagues carried out a systematic review and meta-analysis of existing research on the topic.
Lung function
The Medline, Embase and CINAHL databases were searched from 1/01/00 to 31/01/23 for studies that compared the lung function of individuals with a history of TB with that of healthy controls.
The meta-analysis included data on 75,631 individuals from 15 studies conducted in 17 countries with varying TB incidence and income levels.
The 7,377 TB survivors had an average age range of 11-65 years. Many of the studies were skewed towards a younger population (<50years) from mainly low- and middle-income countries.
Four measures of lung function were included in the analysis: forced expiratory volume in 1 second (FEV1, the volume of air can be forcefully exhaled in one second); forced vital capacity (FVC, the volume of air that can be forcefully exhaled in a single breath); FEV1/FVC ratio; FVC as a percentage of the predicted value (compares the volume to the average of a healthy person of the same age, sex and height).
The findings
The study, which was supported by the charity Breathing Matters, found that, compared to the healthy controls, the participants with prior TB had significantly lower results on all four measures of lung function, with FEV1 more affected than FVC.
Dr Ratnakumar says: “FEV1 was 230 millilitres lower compared to healthy controls and FVC was 140 millilitres lower. A decrease in FEV1 of 100 millilitres is considered clinically significant and is associated with an increased risk of cardiovascular and respiratory disease.”
The results as a whole point to the TB survivors having smaller lungs (restrictive disease) and narrower airways with slower air flow (obstructive disease). This means that the breaths they take are smaller and take longer; breathing is less efficient and less able to respond to increased ventilatory demands such as during exercise.
Analysis of data from five of the studies showed the TB survivors to have 65% higher odds of airflow obstruction (AFO) than the healthy controls.
Lasting impact
The results suggest TB can leave a lasting and widespread impact on the lungs, especially in terms of how the airways are structured. This valuable insight can help guide rehabilitation strategies and, in the longer term, aid in the development of new therapies, say the researchers.
Dr Ratnakumar explains: “Our results strongly indicate that post-tuberculosis lung disease is an under-recognised global challenge – and one that has significant implications for clinical practice and policy.
“The focus, until now, has been on the treatment of acute TB, but even when treatment is successful, individuals can be left with significant lung damage.
“This can cause breathlessness that can affect their ability to work and go about their day-to-day lives and reduces their quality of life.
TB legacy
“This legacy of TB has been overlooked for too long and it is vital it is recognised.
“With an estimated 74 million lives saved through tuberculosis treatment between 2000 and 2020 and a rising life expectancy, there is an urgent need for evidence-based recommendations on the diagnosis, treatment and management of post-tuberculosis lung disease.
“Our study also provides compelling evidence that the long-term care of individuals with post-tuberculosis lung disease should be an explicit component of the WHO’s End TB strategy.”






No comments yet