A new study led by researchers at University of Limerick in Ireland has revealed the ‘most effective’ way to diagnose maternal sepsis, a condition with a devastating global impact.

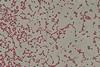
The new study of microbiology specimens used to investigate maternal sepsis has found that placental swabs can provide critical information for guiding antimicrobial treatment.
The findings, described as ‘very significant’ by the research team, have just been published in the highly respected PLOS ONE academic journal.
Maternal sepsis
The study was performed by researchers from University of Limerick (UL) and University Maternity Hospital Limerick (UMHL) and involved the examination of almost 2,000 specimens collected over five and a half years.
Maternal or perinatal sepsis is a well-recognised risk and a condition affecting over 20 million women and causing 17,000 deaths annually.
Identifying the causative agents can be challenging, however. Blood cultures, the gold standard for diagnosis, often have low positivity rates. Other samples, such as vaginal swabs, offer limited clinical value.
This unique new study was led by Professor Colum Dunne, Head of School and Foundation Chair and Director of Research at the UL School of Medicine and performed by a team of researchers from UL and UMHL.
Septic screen
The team retrospectively analysed the bacterial culture results of a number of different specimens that were collected as part of a ‘septic screen’, which detects bacteria that may cause maternal infections and can lead to sepsis. These specimens were: blood, urine, throat swabs, vaginal swabs and placental swabs.
“Maternal sepsis may occur during pregnancy or when a C-section incision, tear or other wound from childbirth becomes infected in the days or weeks after giving birth,” explained Professor Dunne.
“This study provides new information on how sepsis can be detected, and the organisms involved identified early, so that the best approach to successful treatment can be selected.”
Inconsistent guidelines
Professor Dunne explained that national and indeed international guidelines are “not consistent” in their recommendations for diagnosing of maternal infections, and there is very little information available in the scientific literature regarding the use of placental swabs.
“By looking at the results of each of these specimens from 430 women, they could be compared to determine which detected the highest pathogen numbers and, in this study, placental swabs were found to be the most effective,” Professor Dunne explained.
“These findings are very significant as these swabs are not always tested in hospitals. Due to this, important information that could be used in treatment choice for these infections could be missed.”
Diagnostic tool
James Powell, a Surveillance Scientist at University Hospital Limerick and one of the lead authors, said: “I am delighted to be a part of the team that conducted this research, and it was a great honour to be able to present our findings at the European Congress of Clinical Microbiology and Infectious Diseases, in Copenhagen, Denmark.”
Professor Roy Philip, a Consultant Neonatologist and Paediatrician at the Division of Neonatology, Department of Paediatrics, University Maternity Hospital Limerick, and Adjunct Associate Clinical Professor of neonatology at UL, explained: “Placental microbial analysis remains a relatively unexplored diagnostic tool in the management of perinatal sepsis, and we hope our research enhances the clinical awareness.”
Professor Nuala O’Connell, Consultant Microbiologist and Adjunct Associate Clinical Professor of Microbiology at UL, added: “The value of sending placental swabs for microbiological analysis as part of a septic workup is under-recognised.
“This study will augment the medical literature in the areas of both maternal and neonatal sepsis diagnostics and thereby assist with antimicrobial stewardship.”






No comments yet