Researchers at Flinders University have taken a major step in the field of wound care by using plasma technology to ‘transform’ Spirulina microalgae into ultrathin bioactive coatings.
The innovative approach uses argon atmospheric plasma jet technology to transform Spirulina maxima, the blue-green microalgae, into bioactive coatings which can tackle bacterial infections while also promoting faster wound healing and applying potent anti-inflammatory properties.
Chronic wounds
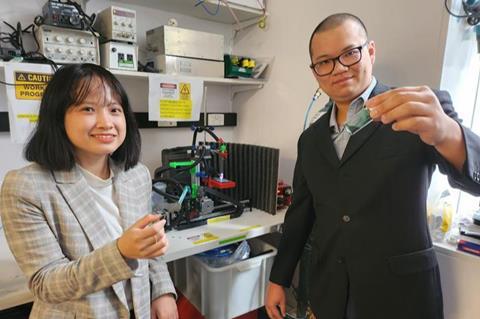
“This holds promise, especially for the treatment of chronic wounds, which often pose challenges due to prolonged healing times,” says Dr Vi Khanh Truong, from the Flinders University Biomedical Engineering Laboratory.
“This novel approach could reduce the risk of toxic reactions to silver and other nanoparticles and rising antibiotic-resistance to common commercial coatings used in wound dressings.”
The latest development, published in the high-impact international peer-reviewed nanotechnology journal Small, reveals a new patented plasma-assisted technology which sustainably processes Spirulina maxima biomass into bioactive ultrathin coatings that can be applied to wound dressings and other medical devices which accelerate healing, modulate inflammation and even protect patients from infection.
Adaptable technique
The new technique could be readily applied to other types of natural supplements, adds Dr Truong.
“We are using the plasma coating technology to turn any type of biomass – in this case Spirulina maxima – into a more sustainable high-end coating.
Extract of S. maxima is often used as a protein supplement and to treat skin disorders such as eczema, psoriasis and other conditions. Researchers say the new plasma technology is the first of its kind and could be a game-changer for wound healing around the world.
Antimicrobial resistance
The WHO has warned that antimicrobial resistance is one of the top public health threats facing humanity in the 21st century. Associated with the death of close to 5 million people in 2019, it is forecast to cost world economies upwards of US$1 trillion by 2050 if no action is taken.
Multiple genetic changes in common bacteria, such as Staphylococcus aureus and Pseudomonas aeruginosa, can lead them to become resistant to multiple antibiotics, forming ‘superbugs’.
Co-author of the new study, Matthew Flinders Professor Krasimir Vasilev, NHMRC Leadership Fellow, says the technology offers a better solution to current commercial applications, including gold and copper coatings, which will be an important tool to combat antibiotic resistance.
“This new plasma-facilitated downstream processing can improve extraction and purification of useful compounds from biomass without the need for harmful solvents and a lot of energy input,” says Professor Vasilev, Director of the Flinders Biomedical Nanoengineering Lab.
“We are now seeking avenues for commercialisation of this unique technology.
Market advantage
“Currently there are no commercial wound dressings that simultaneously fight and protect from infection, favourably modulate inflammation and stimulate healing.
“We believe that the technology will offer a market advantage to medical wound dressing manufacturers and, by reaching the hospitals, make a difference to healthcare and patients.”
The Covid-19 pandemic increased the need for non-toxic, biocompatible, biostable antimicrobial coatings, a market projected to increase in value from almost US$4 billion to $6.8 billion within five years.
Acknowledgements: The research received funding from the ARC, NHMRC and Flinders Foundation. This work is part of a Master of Biotechnology thesis by Ms Tuyet Pham.







No comments yet