Scientists have unveiled a new tool for studying the highly variable traits that allow malaria parasites to stick to red blood cells and evade the immune system.
The study, published as a Reviewed Preprint in eLife, introduces an important approach for generating Plasmodium falciparum parasite lines that express specific variants of a sticky adhesin molecule, according to eLife’s editors. They say that it also provides compelling evidence for an innovative and rigorous platform that can explore how malaria causes disease.
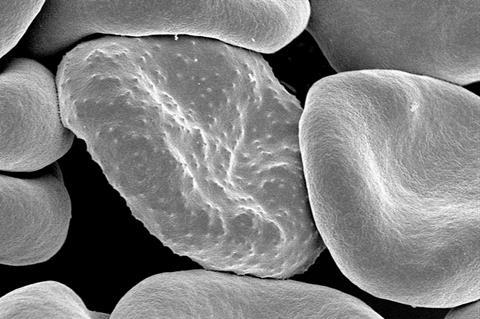
The ability of the human malaria parasite to stick to red blood cells – called cytoadhesion – allows it to escape clearance by the immune system and cause the build-up of infected red blood cells in major organs, with life-threatening consequences.
Protein family
Cytoadhesion is facilitated by members of a protein family called ‘P. falciparum erythrocyte membrane protein 1’ – or PfEMP1. Each parasite produces only one type of PfEMP1 at any time, governed by its genes, and it can switch between different forms of PfEMP1 to avoid immune recognition.
“A key problem in studying PfEMP1 is that when you grow malaria in the lab, it results in a population of parasites with diverse PfEMP1 proteins with different properties,” explains lead author Jakob Cronshagen, at the time of the study a doctoral student shared between the Bruchhaus and Spielmann labs at the Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany. “Researchers have tried to select for parasite strains producing certain PfEMP1 proteins, or use antibodies to study them, but this has proved challenging.”
READ MORE: Human antibodies could prevent the malaria parasite from causing life-threatening infections
READ MORE: Scientists uncover structure of hemezoin crystals crafted by malaria parasite
To address this, Cronshagen and colleagues used a method called selection linked integration (SLI), in which an antibiotic is used to selectively enrich parasites containing a specific type of protein. This generated parasites that predominantly make one specific PfEMP1 protein, enabling the team to study facets of PfEMP1 biology in more detail.
Tracking movements
For example, previous work had indicated that mutants of different proteins involved in trafficking of PfEMP1 block its transport at different points as it moves to the surface of red blood cells. The authors used their new SLI method to obtain parasites all expressing a tagged version of PfEMP1, allowing them to track its movements. Moreover, the authors used their new method to study the PfEMP1 ‘proxiome’ – that is, the group of proteins that most closely collaborate with PfEMP1 during the development of malaria infection – and in addition to confirming known relationships, they identified two new proteins involved in the cytoadhesion process.
Another essential requirement for studying these pathogenic PfEMP1 proteins is to allow the parasite to switch between PfEMP1 variants as it would naturally do during an evolving malaria infection. The team tested this by removing the antibiotic used to select for the specific PfEMP1, and found that the parasites evolved from a uniform population all predominantly making the same PfEMP1, to a diverse population making a range of PfEMP1 variants.
Malaria pathology
“The way in which PfEMP1 functions and how it is neutralised by human antibodies are increasingly being uncovered on a structural level and are essential for understanding malaria pathology and immune responses in patients,” concludes senior author Tobias Spielmann, Research Group Leader at the Bernhard Nocht Institute for Tropical Medicine. “The straightforward capacity to generate cell-adherent parasite lines uniformly expressing a single PfEMP1 of interest will open up new approaches to block these pathogenicity proteins as a new therapeutic strategy in malaria.”






No comments yet