Research analysing European survey data from 113,884 men who have sex with men (MSM) and published in Eurosurveillance indicates that while most MSM have a basic understanding of viral hepatitis, only 44% report having been vaccinated against both hepatitis A and B.

The data highlight notable immunisation gaps despite available vaccination and recommendations. Strong public health support and creating an open environment that enables MSM to follow recommendations will be crucial to reduce outbreaks among MSM and eliminate hepatitis B.
READ MORE: Study reveals vaccination patterns among LGBTQ+ adults in New Jersey and New York
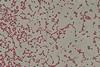
Men who have sex with men are more likely to get infected with viral hepatitis, with risks being exacerbated by stigma and discrimination, which can affect access to healthcare services. While sex between men is the second most commonly reported route of acute hepatitis B virus infection in Europe, only three quarters of European countries (32/42) recommend vaccination against hepatitis B specifically for MSM. Outbreaks of hepatitis A have been reported among MSM worldwide, including a large multi-country outbreak in Europe in 2016–2018. However, just under half of European countries (19/43) recommend hepatitis A vaccination for MSM.
Vaccination uptake and basic knowledge
The two studies looked at data from 113,884 participants in the WHO European Region from the European MSM Internet Survey 2017 (EMIS-2017) with Brandl et al. analysing vaccination uptake data, and Burdi et al. reviewing basic knowledge about hepatitis A and B. EMIS-2017 was an anonymous, open access internet survey carried out between late 2017 and early 2018 on the sexual health of MSM. Both studies looked at data from respondents that were above the age of consent in their country, identified as cis or trans men, and indicated that they were attracted to men and/or had sex with men.
Brandl et al. reviewed data on self-reported hepatitis A and B vaccination status by age, education, financial coping, settlement size, openness about sexual orientation, migration history and diagnosis with hepatitis C or HIV. The study also compared these data against information on national hepatitis A and B vaccination recommendations.
Only 48% of respondents reported being vaccinated against hepatitis A, and 53% against hepatitis B, with significant differences in uptake between countries. Reported vaccination rates for either disease were higher among respondents that were more open about their sexual orientation (‘outness’), and in countries where vaccination for that disease was specifically recommended for MSM. Participants were more likely to report being vaccinated if they were older, living in bigger cities, more financially comfortable, or had been diagnosed with hepatitis C and/or HIV.
Viral hepatitis
Burdi et al. looked at the basic knowledge on viral hepatitis and hepatitis vaccination, which may correlate with higher vaccination uptake. Basic knowledge was defined as correctly identifying at least 4 out of 5 statements related to hepatitis in EMIS-2017. Researchers also collected data on sociodemographic characteristics, history of hepatitis C and/or HIV diagnosis, sexual orientation disclosure at the last sexually transmitted infection (STI) test, and outness.
While two thirds of respondents (68%) demonstrated basic knowledge, there was significant disparity among MSM in Europe. Respondents who were older, had a history of hepatitis C and/or HIV diagnosis, were out or had disclosed their sexual orientation at their last STI test were more likely to have basic knowledge. Knowledge was also higher among those who had been vaccinated against viral hepatitis or were immune due to a previous infection. Of the vulnerable, not vaccinated or immune respondents, 58% and 62%, respectively, reported not having been offered a vaccine for hepatitis A or B.
While there were national differences, individual factors played a larger role in reported knowledge levels about viral hepatitis.
Targeted public health action
Both studies highlight the importance of actively recommending vaccination against both hepatitis A and B to MSM, with Brandl et al. also pointing to the benefits of national recommendations for MSM and offering the vaccines for free or with a co-payment. Burdi et al. also suggest improving access to information among younger MSM in smaller settlements with a low level of education, and poorer financial resources.
Researchers for both studies emphasised the crucial role of a supportive, accepting climate to encourage openness, facilitate targeted public health action, and improve health outcomes for MSM.






No comments yet