In a pioneering study, researchers have developed a poly (L-lactic acid) (PLLA) nanofibrous membrane enhanced with curcumin and silver nanoparticles (AgNPs), aimed at improving the healing of diabetic wounds. This advanced dressing targets critical barriers such as inflammation, oxidative stress, and bacterial infections, which hinder the recovery process in diabetic patients. The study’s results reveal a promising therapeutic strategy that could revolutionize care for diabetes-related wounds.
Diabetic wounds are notoriously challenging to heal, with prolonged inflammation and a high risk of infection. Traditional treatments generally offer only passive protection and fail to dynamically interact with the wound environment. The creation of bioactive dressings like the poly (L-lactic acid) (PLLA) nanofibrous membranes incorporated with AgNPs and curcumin (PLLA/C/Ag) membranes signifies a crucial shift towards therapies that actively correct imbalances in the wound healing process, offering a more effective solution for managing diabetic wounds.
Infused membranes
Published (DOI: 10.1093/burnst/tkae009) in Burns & Trauma on June 5, 2024, this research by a team from Mudanjiang Medical University and allied institutions assesses the effectiveness of PLLA nanofibrous membranes. Infused with curcumin and silver nanoparticles, these membranes are designed to substantially enhance the healing processes in diabetic wounds by targeting fundamental issues like excessive inflammation and infection.
READ MORE: Wound treatment gel fights the battle against antibacterial resistance
READ MORE: Engineered nanovesicles from activated neutrophils show promise in treating infected wounds
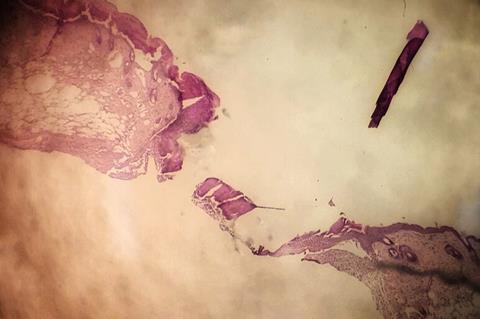
This research centered on developing PLLA/C/Ag nanofibrous membranes through air-jet spinning, achieving a consistent fiber distribution essential for effective therapeutic delivery. The membranes boast dual benefits: antioxidant properties that reduce harmful reactive oxygen species in wound environments and potent antibacterial activity that decreases infection risks.
In vivo tests on diabetic mice demonstrated the membranes’ capability to promote crucial healing processes such as angiogenesis and collagen deposition. These findings illustrate that PLLA/C/Ag membranes not only protect wounds but also actively support and expedite the healing process, marking them as a significant therapeutic innovation for diabetic wound management with potential for broader chronic wound care applications.
Diabetic wound care
Dr. Yanhui Chu, a principal investigator of the study, highlighted the importance of these developments: “The PLLA/C/Ag membranes are a significant breakthrough in diabetic wound care. Their ability to effectively modulate the wound environment and enhance healing could establish a new standard in treatment, providing hope to millions affected by diabetes-related complications.”
The deployment of PLLA/C/Ag nanofibrous membranes in clinical environments could transform the treatment of diabetic wounds, offering a more active and effective approach. Beyond diabetes management, this technology has the potential for extensive applications in various chronic wounds, paving the way for future breakthroughs in bioactive wound dressings. This study not only progresses our understanding of wound management but also paves new paths for developing adaptive treatments for complex wound scenarios.




No comments yet