A research group at the University of Basel, Switzerland, has discovered that the bacterial pathogen that causes cholera forms a novel type of bacterial community on immune cells: an aggressive biofilm that is lethal for the cells.
The study, recently published in the journal Cell, provides new insights into the infection strategies of pathogens.
Many bacteria adopt a fascinating defense strategy by forming communities on surfaces, known as biofilms. Bacterial biofilms are intrinsically tolerant to antibiotics and can pose a significant threat in clinical settings when they colonize implants, catheters, or surgical instruments. This colonization enables pathogens to infiltrate our body and trigger infections that are difficult to combat by the immune system and with antibiotics.
Biofilms on the attack
Previously, it was assumed that bacteria form biofilms to defend and protect themselves. The research team, led by Prof. Knut Drescher at the Biozentrum, University of Basel, has now demonstrated that bacteria form biofilms on the surface of immune cells. This previously unknown type of community differs from already known bacterial biofilms not only in its structure, but also in its function: instead of serving a protective purpose, this biofilm is an aggressive trait.
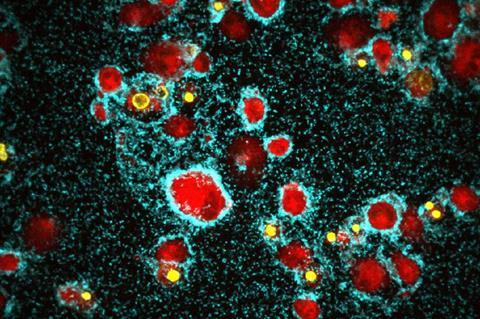
Drescher’s team has discovered this novel type of biofilm in the cholera-causing pathogen Vibrio cholerae. This bacterium colonizes various immune cells in the human host.
To better understand biofilm formation on immune cells, the researchers focused on a certain type of phagocytic cells, so-called macrophages.
Attaching to macrophages
“Bacteria that accidently encounter a macrophage attach to the cell’s surface using a kind of a ‘feeler’,” explains first author Lucia Vidakovic. “Subsequently, the bacteria start to divide and intertwine their feeler-like appendages.”
The structure of the extracellular matrix of this type of biofilm is thus fundamentally different from previously known ones, in which bacteria are typically embedded within a slimy matrix consisting of sugars and proteins.
Over time, the biofilms produced by the cholera pathogen completely encase macrophages, leading to cell death.
“The bacterial community actively attacks and kills the immune cells. However, we initially didn’t understand the exact mechanism,” says Vidakovic. “To solve this puzzle, we meticulously investigated all 14 known toxins produced by the cholera pathogen and could finally identify the hemolysin as the culprit.”
Toxin forming pores
This toxin forms pores in the protective membrane of the immune cells, thus killing them.
Cholera is a life-threatening infectious disease that causes severe diarrhoea. As humans are the only host of the cholera-pathogen, the scientists established a human intestinal organoid model. Using this model, they could demonstrate that Vibrio cholerae is able to form lethal biofilms on macrophages after colonizing and disrupting the human intestinal barrier.
“This novel strategy of attack, employed by the bacteria, can significantly affect the progression of the cholera infection,” adds Knut Drescher. “In a next step, we aim to explore whether other pathogens also form such aggressive biofilms. Deciphering the strategies of bacterial pathogens is crucial for the development of new approaches to fight them.”
The study is part of the National Centre of Competence in Research (NCCR) “AntiResist” and was conducted in collaboration with the École Polytechnique Fédérale de Lausanne. The aim of this research network is the discovery of new antibiotics and the development of novel strategies to combat antibiotic-resistant pathogens.






No comments yet