In recent years, physicians and scientists in parts of Brazil where visceral leishmaniasis (VL) is endemic have seen rising numbers of cases of co-infection by Leishmania infantum and Crithidia, also a protozoan but hitherto believed to be a mosquito parasite that cannot infect humans or other mammals. Accurate diagnosis is hindered by a lack of simple specific tests.
To accelerate and facilitate detection of the pathogens involved, supporting appropriate decisions regarding treatment, researchers at the Federal University of São Carlos (UFSCar) have developed a PCR test which analyzes the genetic material in the sample and produces a result in less than two hours. An article on the study was published in the journal Tropical Medicine and Infectious Disease.
Neglected disease
Leishmaniasis is a neglected disease and is considered a global public health problem. Brazil reports more than 3,500 cases per year, according to the Health Ministry, or 93% of all cases in Latin America. The disease caused 165 deaths in Brazil in 2020.
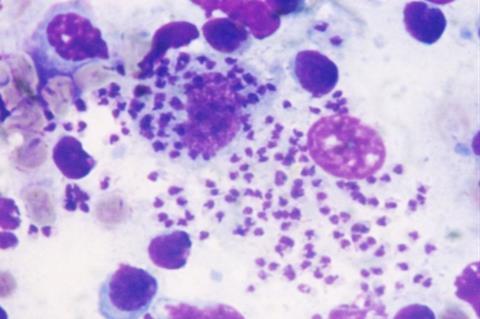
VL is the most severe form of the disease, affecting the spleen, liver, bone marrow and lymph nodes, and can be lethal if it is not correctly treated or is misdiagnosed. The main agent of VL is L. infantum.
The study was funded by FAPESP via nine projects.
The novel method is an advance on the usual diagnostic technique. In the study, it was highly accurate in identifying and quantifying L. infantum and Crithidia in samples obtained in vitro or collected from human hosts as well as dogs, cats and insects by means of skin biopsies or bone marrow aspiration.
Direct from vectors
“Although there are other molecular methods for identifying species, they require DNA sequencing of the sample, which is laborious, slow and expensive. Our test analyzes the parasite’s genetic material directly from vectors and human or animal tissue,” said Sandra Regina Costa Maruyama, last author of the article and a professor of evolutionary genetics and molecular biology at UFSCar.
Unlike the quick tests used by health clinics and pharmacies, which do not detect pathogens directly but identify the relevant antibodies, the researchers designed their dye-based quantitative PCR assay on the basis of targeted sequences from L. infantum and Crithidia in experimental and clinical samples. A test had to be performed first to detect the former parasite, followed by another to identify the latter.
“The targets resulted from our analysis of the two species’ genomes. Our most recent study showed specificity in different sample types. The test can now be optimized to show in a single reaction whether the infection was caused by L. infantum, Crithidia or both,” Maruyama said.
The test can be performed by any diagnostic laboratory capable of performing qPCR tests (now more widespread following the COVID-19 pandemic). It can also be used in epidemiological research, parasite load monitoring, and treatment follow-up.
Co-infection cases
The study involved analysis of 62 parasites isolated from VL patients’ tissues, with 51 testing positive for Crithidia. In addition, bone marrow co-infection by Crithidia and L. infantum was identified in two new cases of VL in Brazil. In May the group published an article on a case of severe VL in which both species were detected.
According to Maruyama, beyond the efficacy of the test, the results show that infection by Crithidia is more frequent than has hitherto been supposed, and that co-infection by both protozoans appears to occur above all in the most severe cases.
“We don’t yet understand the clinical implications of the presence of Crithidia in cases of VL, but we suspect that co-infection exacerbates the disease or prevents patients from responding to the recommended treatment for L. infantum,” she said. “Identifying the species of parasite correctly ensures that appropriate measures can be taken quickly to prevent progression of the patient’s clinical condition, potentially reducing mortality. It also points to the possible development of more specific drugs and treatments in future.”







No comments yet