The number of infectious syphilis diagnoses has reached a new high over the past decade, with an 184.4% rise in reported cases between 2013 and 2023, according to a report from UK Health Security Agency published last year. This has also become the highest recorded level since the 1940s. Syphilis infection, once in decline, has made an alarming comeback and once again raises serious public health concerns.
What is syphilis? Transmission, development, and symptoms
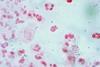
Sexually Transmitted Infections (STIs) remain to be one of the significant global challenges. According to the WHO, there are over 1 million STIs daily, including gonorrhoea (Neisseria gonorrhoeae), chlamydia (Chlamydia trachomatis) and trichomoniasis (Trichomonas vaginalis). Amongst these, syphilis is an STI caused by the bacterial pathogen, Treponema pallidum. It is mostly transmitted through contact with lesions during sexual activities, and through the placenta during pregnancy, leading to babies being born with syphilis (congenital syphilis). Transmissions occur typically up to 2 years after infection.
Normally, several stages of symptoms for syphilis can take place, where clinical features typically occur after 21 days of exposure, with a period of 10-90 days incubation. The primary syphilis infection includes painless and round ulcers around the regions of the mouth, vagina or rectum. If syphilis remains untreated within 6-8 weeks, it will progress to secondary syphilis, which is characterised by a non-itchy rash with mucous white/grey lesions in warm and moist areas, commonly known as condyloma lata. Some complications consist of lymphadenopathy (swelling of the lymph nodes) and occasionally neurologic or ocular manifestations. Primary and secondary syphilis may occur concurrently, which is most likely the case for patients with HIV infection. The risk of contracting HIV can increase by two-fold with existing syphilis infections. At the latent stage of the infection, clinical symptoms are no longer manifested but receive positive serological test results. This could further progress to systemic infection (tertiary syphilis), with inflammatory lesions affecting deeper tissues after years of untreated infection.
Congenital syphilis caused by vertical transmission from mother to foetus is the second-most common cause of preventable global foetal loss after malaria. Syphilis infection during pregnancy could result in complications with profound impacts, contributing to miscarriages, stillbirths, neonatal deaths, low birth weight or even infants with congenital syphilis.
Diagnosis of syphilis mainly relies on clinical history, serological testing and/or direct detection of the pathogen T. pallidum. However, despite the fact that there is currently no diagnostic test for congenital syphilis, maternal serology and treatment for syphilis can be used for disease evaluation.
In spite of the multiple stages of infections, congenital syphilis is still treatable through timely antenatal screenings. The adverse outcomes of foetal syphilis may be averted by the treatment of multiple doses of intravenous benzathine penicillin G (BPG) injection during early pregnancy. This is considered the first line of therapeutic treatment and the only recommended treatment for congenital syphilis, as per WHO guidelines. Other antibiotics, such as ceftriaxone, doxycycline or azithromycin can also be used as second-line treatment.

The current scale of the problem
A surge in adult syphilis and congenital syphilis was reported during the COVID-19 pandemic. The rate of congenital syphilis cases was 523 cases per 100,000 live births, while there were an estimated 700,000 cases worldwide. A total of 230,000 deaths were recorded for congenital syphilis-associated deaths in 2022. Of those infants clinically diagnosed with congenital syphilis, only less than 10% of women were positively tested and received appropriate treatment. There was an increase of 9.4% in diagnosed cases of infectious syphilis between 2022 and 2023, which set the highest annual record since 1948. Screening for sexual health has also increased by 8.3%.
According to a CDC report, reported cases of congenital syphilis were 10 times higher in 2022, compared to 2012, and reached the highest number since the 1950s. During the late 1990s, due to the fear of HIV in the U.S., screening of STIs and sexual behaviour awareness were at their peak. Syphilis was thereby nearly eradicated in 1999. However, syphilis cases continued to rise after the millennium and reached a spike in infections after the pandemic. This is largely attributed to the lack of screening and treatment whilst the population was undergoing self-isolation. The increasing population of gay, bisexual, and other men who have sex with men (GBMSM) has also contributed to the significant rise in syphilis cases.
The impact of socioeconomic factors on congenital syphilis prevalence
WHO Global Health Sector has once established an elimination goal to maintain a level of 50 congenital syphilis cases per 100,000 live births per country, which resulted in a marginal drop in incidence rate amongst African regions. Brazil accounted for the most congenital syphilis cases in the Americas. Based on the data collected in the Western region of the Brazilian Federal District alone, by 2021, the number of congenital syphilis cases was recorded to be 33 times higher than the target of 50 cases per 100,000 live births set by the WHO for the elimination of vertical transmission. In Brazil in 2023, 91% of pregnant women with antenatal care were tested for syphilis, amongst which 61% received adequate treatment. There was, however, a greater proportional rise in syphilis diagnoses among the heterosexual population (21.8%) than among gay, bisexual, and other men who have sex with men (GBMSM), (7.3%) between 2022 and 2023.
The apparent increasing rate of such incidence is likely attributed to the underestimation of the disease burden due to poor surveillance systems, lack of shared information, and difficulty in detecting asymptomatic infections. On the other hand, although the case rates in high-income countries continue to rise, they remain lower than those in low/middle-income settings. Now, the WHO strategy is aiming to reduce the number of new syphilis cases to 90% by 2030.
Ameliorating the problem
There is an initiative from WHO – the Triple Elimination Initiative, which encourages countries to commit to testing for syphilis, human immunodeficiency virus (HIV), and hepatitis B virus (HBV) during antenatal care to account for any existing epidemiological risk factors.
Increasing the availability of point-of-care testing to pregnant women with syphilis also provides a cost-effective antenatal intervention to reduce syphilis prevalence. Since syphilis and HIV are the major global concerns for STIs, a dual syphilis/HIV rapid diagnostic test, instead of the conventional laboratory test, is recommended as a simple and cheap way of testing to provide maternal care and prevent transmission to babies. As well as the efforts by individual countries in improving healthcare systems, as partner coinfection may also increase complications, there is a need for workshops to raise public awareness, to stop the burden of infections.







No comments yet